Translate this page into:
The unidentified white object

*Corresponding author: Sunanda Nandi, Department of Pediatrics, Strabismus and Neuroophthalmology, Child Sight Institute, Kallam Anji Reddy Campus, Lakshmi Vara Prasad Eye Institute, Hyderabad, India. sunanda.amc@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nandi S, Bhate M. The unidentified white object. J Ophthalmic Res Pract. 2024;2:38-9. doi: 10.25259/JORP_12_2024
A 19-year-old boy presented with the chief complaint of diminution of vision in the left eye since childhood. There is no history of any trauma. Best-corrected visual acuity in the right eye was 20/60 and in the left eye 20/400. The patient was operated on for the left eye congenital ptosis 9 years back, which explains the poor vision in the left eye with the subsequent development of sensory exotropia. On the modified Krimsky test, it was 35 prism diopter (PD) exotropia with 10 PD left hypertropia. The anterior and posterior segments were normal. No inflammatory signs were noted in the palpebral conjunctiva or fornix of the left eye. Neuroimaging gave the evidence of incidental finding of <1 mm small, round hyperintense, and well-defined lesion in the sclera of the left eye suggestive of intraocular foreign body (IOFB), as shown in Figure 1.
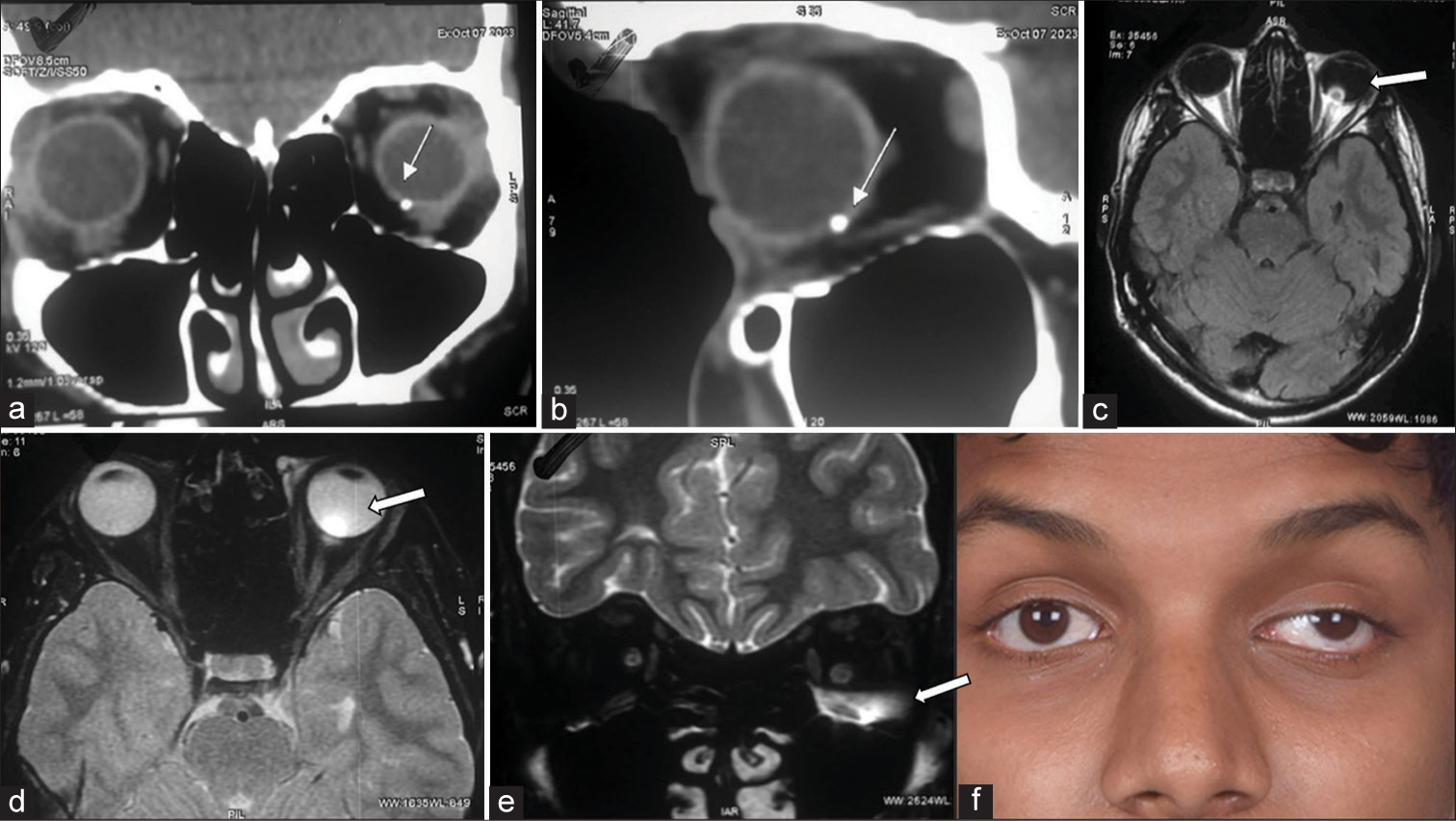
- (a and b) show the round, small, hyperintense foreign body of 1mm in the inferior sclera in the coronal and sagittal section of the CT orbit, respectively (arrows). (c and d) show hyperintense foreign bodies in the axial section of the MRI orbit (arrows). (e) shows hyperintensity involving the inferior rectus muscle of the orbit (arrow). (f) shows the clinical appearance of the patient concerned (arrow).
There were no signs of inflammation of the outer coat of the eye as well as the extraocular muscles; therefore, the patient was given glasses and was asked to follow up after 3 months.
IOFBs may appear as hypointense structures on magnetic resonance imaging (MRI) or computed tomography (CT) scans, depending on their composition and magnetic susceptibility. In cases where IOFBs are incidentally discovered in the sclera, imaging findings may be subtle and require careful evaluation by experienced radiologists and ophthalmologists. MRI is particularly useful for delineating soft-tissue involvement and assessing the extent of ocular trauma, while CT scans provide high-resolution images of bony structures and metallic foreign bodies.[1]
Even asymptomatic IOFBs can lead to significant complications if left untreated. These may include intraocular inflammation (uveitis), secondary glaucoma, retinal detachment, and endophthalmitis. The risk of complications is influenced by various factors, including the size, location, and composition of the IOFB, as well as the presence of associated ocular injuries.[2]
The management of incidentally discovered IOFBs in the sclera depends on several factors, including the patient’s symptoms, visual acuity, ocular examination findings, and imaging characteristics of the foreign body. In cases where the IOFB is small, superficial, and not associated with intraocular inflammation or other complications, a conservative approach with close observation may be warranted. However, larger or deeper IOFBs, or those associated with intraocular inflammation or structural damage, may require surgical intervention for removal and repair of ocular tissues.[3]
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The birmingham eye trauma terminology system (BETT) J Fr Ophtalmol. 2004;27:206-10.
- [CrossRef] [PubMed] [Google Scholar]
- A system for classifying mechanical injuries of the eye (globe). The ocular trauma classification group. Am J Ophthalmol. 1997;123:820-31.
- [CrossRef] [PubMed] [Google Scholar]
- Low rate of endophthalmitis in a large series of open globe injuries. Am J Ophthalmol. 2009;147:601-8.e2.
- [CrossRef] [PubMed] [Google Scholar]