Translate this page into:
Prevalence of pre-operative astigmatism using swept-source optical coherence tomography in patient undergoing cataract surgery

*Corresponding author: Shaik Mohammed Arif Mansoor, Department of Ophthalmology, Choudhury Eye Hospital and Research Centre, Silchar, Assam, India. mansoorarif9@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mansoor SA, Kharibam MD, Acharya M. Prevalence of pre-operative astigmatism using swept-source optical coherence tomography in patient undergoing cataract surgery. J Ophthalmic Res Pract 2023;1:14-8.
Abstract
Purpose:
The purpose of this study was to assess the prevalence of pre-operative astigmatism in patient reporting for cataract surgery using swept-source optical coherence tomography (OCT) in a tertiary care eye hospital.
Methods:
Prospective cross-sectional study in patients undergoing cataract surgery with having age ≥35 years. Ophthalmic biometry was done using swept-source OCT (intraocular lens, IOL Master 700). The various parameters that were studied are axial length, anterior chamber depth, lens thickness, white-to-white measurement, and keratometry (K) (K1-flat K and K2-steep K). Corneal astigmatism was determined by the difference between K2 and K1 reading.
Results:
A total of 310 eyes from 155 patients were evaluated. There were 70 males (45.16%) and 85 females (54.83%). The mean age of study population was 64.43 ± 9.18 years. The mean corneal astigmatism was 0.91D ± 0.67D ranging from 0 to 4.21D. No astigmatism was present in 3 eyes (0.96%), astigmatism with-the-rule was detected in 90 eyes (29.03%), against the rule astigmatism was detected in 167 eyes (53.87%), and oblique astigmatism was found in 50 eyes (16.12%). 214 eyes (69.02%) had corneal astigmatism <1.00D and 96 eyes (30.98%) had corneal astigmatism ≥1.00D.
Conclusion:
The study shows that 30.98% of eyes reporting for cataract surgery had pre-existing corneal astigmatism ≥1.0D and were offered the option of astigmatism correction with toric IOL implantation. The larger majority of eyes 69.02% had corneal astigmatism <1.0D and could be managed with spherical monofocal IOL.
Keywords
Pre-operative corneal astigmatism
Swept-source optical coherence tomography
Ophthalmic biometry
Cataract surgery
INTRODUCTION
The most frequently performed ophthalmic surgery worldwide is cataract surgery, with correction of refractive errors and removal of cataracts at the same time. Cataract surgery has undergone a paradigm shift from being a vision restoration surgery to a refractive surgery with patients demanding no to minimal residual refractive error, postoperatively.[1] Accurate measurement of pre-operative corneal astigmatism has become pertinent to attain a satisfactory refractive outcome. Equally important is the intraocular lens (IOL) power calculation, which is dependent on correct axial length (AL) and anterior chamber depth (ACD) measurement.[2] Studies have shown that a prime cause of reduced vision post-operatively is accountable to corneal astigmatism.[3] Patients can only attain spectacle independence for distant vision if postoperative astigmatism is ≤0.5 Diopters (D).[4]
The latest optical biometer IOL Master 700 (Carl Zeiss) based on swept-source optical coherence tomography (OCT) has been found to be the gold standard for keratometry and AL measurement. It has demonstrated brilliant consistency and agreeability with Pentacam and was found better than IOL Master 500 (Carl Zeiss) and Lenstar 900 (Haag Streit).[5] There have been multiple studies on corneal astigmatism prevailing in patients reporting for cataract surgeries from various parts of the world. The device used for doing keratometry in those studies was Auto-refracto-keratometer,[6] manual keratometry,[7] optical low coherence reflectometry,[8] and partial coherence interferometry.[2,9] One study from China has used IOL Master 700 for evaluating prevailing corneal astigmatism in subjects with high myopia and co-existing cataract.[5] Pre-operative corneal astigmatism in Indian population using swept-source OCT has not been reported. The present study was undertaken to assess the prevalence of pre-operative astigmatism in patients undergoing cataract surgery using swept-source OCT in a tertiary care eye hospital.
METHODS
It was a cross-sectional study and prospective in nature, carried out in a tertiary care eye hospital of South Assam. The study duration was from March 2022 to June 2022. Patients undergoing cataract surgery having age ≥35 years were study participants. Patients underwent comprehensive ocular examination including visual acuity, refraction, slit-lamp evaluation, rebound tonometry, dilated fundus examination, and optical biometry. Patients having corneal disease, pterygium, or a history of previous intraocular surgery were excluded from the study. The study was conducted in accordance with tenets of Declaration of Helsinki. Approval was obtained from the Ethics Committee before onset of the study. Written informed consent from all patients was obtained.
Study device
IOL Master 700 is newer generation non-contact optical biometer using a laser with wavelength of 1055 nm (swept-source technology). AL, ACD, and lens thickness (LT) are all measured using newer swept-source OCT. Telecentric keratometry is utilized to measure corneal curvature aided by reflected light spots from corneal surface.[10]
Case definition
The keratometry (K) values are obtained from the corneal central 2.5 mm in two meridians, namely, K1 or flat K and K2 or steep K. Astigmatism was determined by the difference of K2 and K1 reading. Corneal astigmatism was defined as with-the-rule (WTR) if the steep axis was 90 ± 30°. If the steep corneal meridian lies at 180 ± 30°, it was labeled as against-the-rule (ATR) astigmatism; oblique astigmatism was labeled when the steep meridian was neither WTR nor ATR. No astigmatism was present when the difference between Steep K and Flat K is zero.[5] Optical biometry using IOL Master 700 was done in all cases by two senior technicians.
Statistical analysis
Apart from the demography of the patients, biometric parameters were filled up in Microsoft Excel (Office 2019). SPSS software (version 22.0) was employed for statistical analysis. Data with quantitative variables were expressed as Mean ± Standard Deviation. For the ease of statistical analysis, the subjects were divided into five groups based on distribution of age, namely, >35–50 years, 51–60 years, 61–70 years, 71–80 years, and ≥81 years. Magnitude of corneal astigmatism was divided into five groups, namely, <1.00D, 1.00–1.5D, 1.5–2.0D, 2.0–4.0D, and >4.0D. Both eyes of all patients were included for analysis. Patients having pseudophakia or aphakia in either eye were excluded from the study.
RESULTS
A total of 310 eyes from 155 patients were evaluated. There were 70 males (45.16%) and 85 females (54.83%). Mean age of study population was 64.43 ± 9.18 years. The mean corneal astigmatism was 0.91D ± 0.67D which ranged from 0 to 4.21D. No astigmatism was present in 3 eyes (0.96%), astigmatism WTR was found in 90 eyes (29.03%), against the rule astigmatism (ATR) was found in 167 eyes (53.87%), and oblique astigmatism was found in 50 eyes (16.12%). 214 eyes (69.02%) had corneal astigmatism <1.00D and 96 eyes (30.98%) had corneal astigmatism ≥1.00D. Thus, 30.98% (one-third) of study population were eligible for phacoemulsification with toric IOL implantation. Majority of the subjects, however, could be given good post-operative outcome with monofocal (spherical) lens implantation.
The age group and sex-wise distribution of the biometric profile of our subjects is given in [Table 1]. The age distribution of study population and their mean astigmatism are given in [Table 2]. Magnitude of astigmatism in study population is given in [Table 3]. Pattern of prevailing corneal astigmatism in our subjects is given in [Figure 1]. Age-wise distribution of astigmatism variants is given in [Figure 2]. Mean of pre-operative astigmatism in different age groups is given in [Figure 3].
| Age (years) Sex |
Eyes (n) | AL (mm) Mean±SD | ACD (mm) Mean±SD |
LT (mm) Mean±SD | WTW (mm) Mean±SD |
K1 (D) Mean±SD |
K2 (D) Mean±SD |
ΔK (D) Mean±SD |
|---|---|---|---|---|---|---|---|---|
| >35–50 | ||||||||
| Male | 4 | 24.11±0.5 | 3.63±0.12 | 3.72±0.40 | 12.2±0.63 | 42.84±1.54 | 43.45±1.39 | 0.60±0.15 |
| Female | 16 | 23.45±1.87 | 3.55±0.41 | 3.96±0.60 | 12.03±0.35 | 44.63±1.41 | 45.41±1.48 | 0.76±0.47 |
| 51–60 | ||||||||
| Male | 28 | 23.29±1.06 | 3.33±0.46 | 4.18±0.57 | 11.93±0.28 | 43.99±1.27 | 44.94±1.47 | 0.94±0.73 |
| Female | 49 | 23.09±1.28 | 3.13±0.51 | 4.25±0.56 | 11.84±0.39 | 44.56±1.27 | 45.40±1.22 | 0.84±0.54 |
| 61–70 | ||||||||
| Male | 66 | 23.24±0.97 | 3.23±0.32 | 4.38±0.44 | 12.01±0.37 | 44.04±1.69 | 44.84±1.69 | 0.82±0.57 |
| Female | 74 | 22.71±0.67 | 3.14±0.32 | 4.24±0.43 | 11.94±0.44 | 44.86±1.50 | 45.67±1.67 | 0.83±0.69 |
| 71–80 | ||||||||
| Male | 36 | 23.10±0.79 | 3.22±0.30 | 4.42±0.44 | 11.97±0.45 | 43.91±1.14 | 45.12±1.42 | 1.12±0.86 |
| Female | 25 | 22.77±0.63 | 3.12±0.52 | 4.27±0.43 | 11.97±0.38 | 44.66±1.56 | 45.47±1.68 | 0.81±0.52 |
| ≥81 | ||||||||
| Male | 6 | 22.72±0.33 | 3.03±0.24 | 4.79±0.44 | 11.76±0.13 | 45.26±1.40 | 46.73±1.12 | 1.47±0.56 |
| Female | 6 | 22.39±1.09 | 3.14±0.22 | 4.42±0.17 | 11.68±0.63 | 43.84±2.93 | 45.57±2.57 | 1.73±1.14 |
AL: Axial length, ACD: Anterior chamber depth, LT: Lens thickness, WTW: White-to-white measurement, K: Keratometry, D: Diopters, SD: Standard deviation
| Age group (years) | Number of eyes n (%) |
Mean astigmatism (Mean±SD) |
|---|---|---|
| >35–50 | 20 (6.45) | 0.808±0.43 D |
| 51–60 | 77 (24.83) | 0.878±0.618 D |
| 61–70 | 140 (45.16) | 0.831±0.636 D |
| 71–80 | 61 (19.6) | 1.049±0.762 D |
| ≥81 | 12 (3.87) | 1.604±0.869 D |
SD: Standard deviation
| Astigmatism (Diopters) | Number of eyes=n (%) |
|---|---|
| Zero | 3 (0.96) |
| <1.00 | 211 (68.06) |
| 1–1.50 | 51 (16.45) |
| >1.51–2.00 | 21 (6.77) |
| >2.01–4.00 | 23 (7.41) |
| >4.00 | 2 (0.64) |

- Pattern of pre-operative corneal astigmatism.
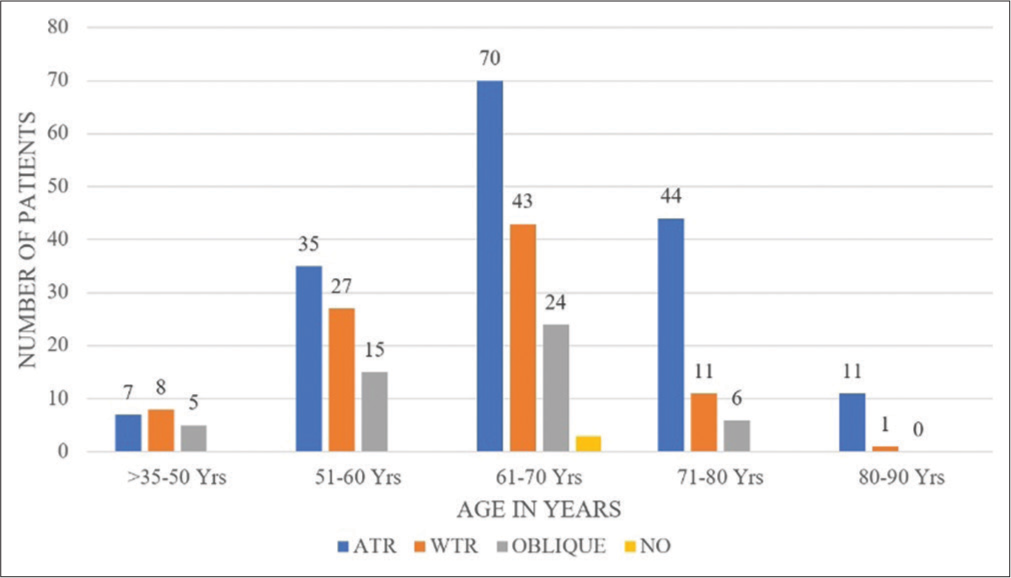
- Distribution of astigmatism according to age groups.
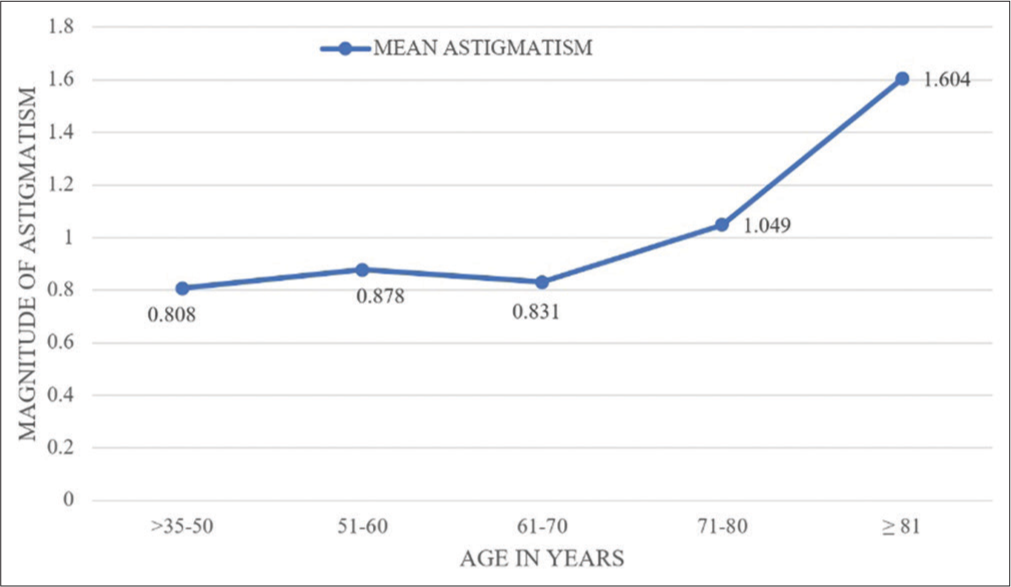
- Mean of pre-operative astigmatism in different age groups.
DISCUSSION
The present study has assessed the prevalence of pre-operative astigmatism in patients reporting for cataract surgery using swept-source OCT in a tertiary care eye hospital. The study population comprised Indians residing in North Eastern part of the country (Assam). PubMed search has not revealed studies done to describe the prevalence of pre-operative corneal astigmatism in Indian population using swept-source OCT. Although, there have been numerous studies to compare the repeatability and accuracy of swept-source OCT (IOL Master 700) with optical low coherence reflectometry (IOL Master 500),[11] Scheimpflug-Placido disk-based tomography,[12] Eyestar 900,[13] Anterion,[14] and Argos.[15]
The reported prevalence of preexisting astigmatism of ≥1.00D in patients undergoing cataract surgeries in the previous studies ranges from 30.8% to 66.9%.[2,5-9] In our study, the prevalence of astigmatism of ≥1.00D was found to be 30.98%. This is almost similar to that found by Rashid et al. (30.4%)[6] and Joshi and Jadhav (32.5%)[16] but was much less than other studies done in North India (40.49%),[8] North East India (45.55%),[2] China (51.5%),[5] United Kingdom (42%),[17] and Nigeria (66.9%).[7]
Mean age of our subjects was 64.43 ± 9.18 years. It was similar to that reported by Natung et al. (64.04 ± 10.81 years),[2] Rashid et al. (61.9 ± 8.1 years),[6] and Isyaku et al. (60.8 ± 12.7 years),[7] but higher than that reported by Sharma et al. (59.12 ± 15.19 years).[8] The mean age of subjects reported by Day et al. was rather higher (79 ± 7 years).[16]
Mean corneal astigmatism in the present study was 0.91D ± 0.67D. It was less than that reported by Rashid et al. 1.17 ± 0.75D,[6] Isyaku et al. 1.16D,[7] and Sharma et al. 1.17 ± 1.15D.[8] Tan et al. have reported mean astigmatism of 1.20 ± 0.83D in subjects with high myopia. However, the mean astigmatism reported by him in the control group was 0.93 ± 0.69D,[5] similar to the present study.
ATR astigmatism was found to be more commoner (53.87%) than WTR astigmatism (29.03%) in the present study. This was similar to that reported by Sharma et al. (51.7% vs. 29.83%),[8] Joshi and Jadhav (44.6% vs. 20.7%),[16] and Day et al. (51.7% vs. 29.83%).[17] Distribution of types of astigmatism according to age groups showed that WTR astigmatism was slightly more (n = 8) than ATR astigmatism (n = 7) in the age group >35–50 years in our study. However, in all the other age groups, ATR astigmatism was more commoner than WTR astigmatism [Figure 2]. However, the study reported by Tan et al. on high myopia patients, having relatively less age (<60 years), WTR astigmatism was found in 63.1% study population.[5] Oblique astigmatism in our study was found in 16.12%, similar to Natung et al. (18.4%)[2] and Sharma et al. (15.59%),[8] and lesser than Joshi and Jadhav (32%).[16]
The strength of our study is, till date there has been no report on prevalence of pre-operative corneal astigmatism using swept-source OCT (IOL-Master 700). The previous reported studies from India were done using LensStar LS9000[8] and IOL Master 500.[2] We have also included data from both eyes of all patients, which was not consistently done in the reported literature.[17] Data from both eyes gives a better insight into the biometric parameters of the population.
Limitations of our study is, the correlation between different parameters of our study, namely, age with AL, ACD, LT, white-to-white measurement, K1, and K2 has not been done. We intented to report the prevalence of corneal astigmatism in patients coming for cataract surgery. The present study is limited to a hospital-based study from North East India (Assam) that may not be representative of the community.
CONCLUSION
The study shows that 30.98% of eyes undergoing cataract surgery had pre-existing corneal astigmatism ≥1.0D and were offered the option of astigmatism correction with toric IOL implantation. The larger majority of eyes 69.02% had corneal astigmatism <1.0D and could be managed with spherical monofocal IOL. This study also highlights the fact that the prevalence of corneal astigmatism in Indian population varies in different parts of the country.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Changes in corneal astigmatism among patients with visually significant cataract. Can J Ophthalmol. 2014;49:297-303.
- [CrossRef] [PubMed] [Google Scholar]
- Ocular biometry characteristics and corneal astigmatisms in cataract surgery candidates at a tertiary care center in NorthEast India. Indian J Ophthalmol. 2019;67:1417-23.
- [CrossRef] [PubMed] [Google Scholar]
- Toric intraocular lenses in the correction of astigmatism during cataract surgery: A systematic review and meta-analysis. Ophthalmology. 2016;123:275-86.
- [CrossRef] [PubMed] [Google Scholar]
- Approaches to corneal astigmatism in cataract surgery. Curr Opin Ophthalmol. 2013;24:30-4.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of preoperative corneal astigmatism using swept-source optical biometry in Chinese cataract surgery candidates with high myopia: A prospective, comparative observational study. Ann Transl Med. 2021;9:618.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Pre-existing corneal astigmatism in age related cataract patient. Faridpur Med Coll J. 2013;8:2-4.
- [CrossRef] [Google Scholar]
- Preoperative corneal astigmatism among adult patients with cataract in Northern Nigeria. Indian J Ophthalmol. 2014;62:1094-5.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of astigmatism in patients undergoing cataract surgery at a tertiary care center in North India. Clin Ophthalmol. 2021;15:617-22.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of corneal astigmatism before cataract surgery in Western Indian Population. Med J Armed Forces India. 2018;74:18-21.
- [CrossRef] [PubMed] [Google Scholar]
- An evaluation of the IOLMaster 700. Eye Contact Lens. 2018;45:117-23.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of IOL-master 700 and IOL-master 500 biometers in ocular biological parameters of adolescents. Int J Ophthalmol. 2021;14:1013-7.
- [CrossRef] [PubMed] [Google Scholar]
- Repeatability and comparability of keratometry measurements obtained with swept-source optical coherence and combined dual Scheimpflug-Placido disk-based tomography. J Cataract Refract Surg. 2020;46:1637-43.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of biometry measurements and intraocular lens power prediction between two swept-source based OCT biometers. J Cataract Refract Surg. 2023;49:460-6.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison study of the two biometers based on swept-source optical coherence tomography technology. Diagnostics (Basel). 2022;12:598.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative analysis of 2 swept-source optical coherence tomography biometers. J Cataract Refract Surg. 2019;45:1124-9.
- [CrossRef] [PubMed] [Google Scholar]
- Frequency of corneal astigmatism in patients presenting for senile cataract surgery at a teaching hospital in Indian Rural Population. Asia Pac J Ophthalmol (Phila). 2020;9:126-9.
- [CrossRef] [PubMed] [Google Scholar]
- Distribution of preoperative and postoperative astigmatism in a large population of patients undergoing cataract surgery in the UK. Br J Ophthalmol. 2019;103:993-1000.
- [CrossRef] [PubMed] [Google Scholar]