Translate this page into:
Intravitreal anti-vascular endothelial growth factor (bevacizumab) in nanophthalmic exudative macular detachment – A new treatment modality

*Corresponding author: Satyen Deka, Department of Retina, ASG Eye Hospital, Guwahati, Assam, India. drsatyen@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Deka S, Singh V. Intravitreal anti-vascular endothelial growth factor (bevacizumab) in nanophthalmic exudative macular detachment – A new treatment modality. J Ophthalmic Res Pract 2023;1:89-92. doi: 10.25259/JORP_18_2023
Abstract
Nanophthalmic exudative macular retinal detachment is a known entity, till now the established treatment modality is Scleral Resection. This brief communication suggests a successful new modality of non-surgical, less invasive treatment approach of intravitreal anti-vascular endothelial growth factor in case of exudate macular detachment related to nanophthalmos.
Keywords
Nanophthalmos
Intravitreal
Bevacizumab
Exudative
Detachment
INTRODUCTION
Nanophthalmos is an uncommon disease having eyes with short axial length and scleral thickening. Corneal diameter is mildly reduced and lens size is normal or mildly increased. Patients with nanophthalmos usually have hypermetropia ranging from 10 to 20 diopters (D) This condition is induced by a developmental arrest of ocular growth. Brockhurst had described the association of nanophthalmos with uveal effusion.[1,2]
Uveal effusion syndrome (UES), a rare condition, typically presents with exudative detachment of ciliary body, choroid, and retina because of congenital anomaly of sclera. There is disorganization of collagen fibers in sclera, and increased scleral thickness which decreases drainage of posterior segment by vortex veins compression.[1-3]
Till now treatment is only surgical, in the form of partial/full thickness sclerotomies and vortex vein decompression. A recent study has shown that interleukin (IL)-6 and IL-8, vascular endothelial growth factor (VEGF) levels in aqueous humor are increased in patients with UES. This supports the hypothesis that choroid capillaries in patients with UES have abnormal permeability.[4-6] Hence, we decided to evaluate the effect of anti-VEGF as a treatment option in such patients. We report a case with bilateral exudative macular detachment in nanophthalmic eyes, in which we used anti-VEGF injections, which resulted in resolution of exudative macular detachment.
CASE REPORT
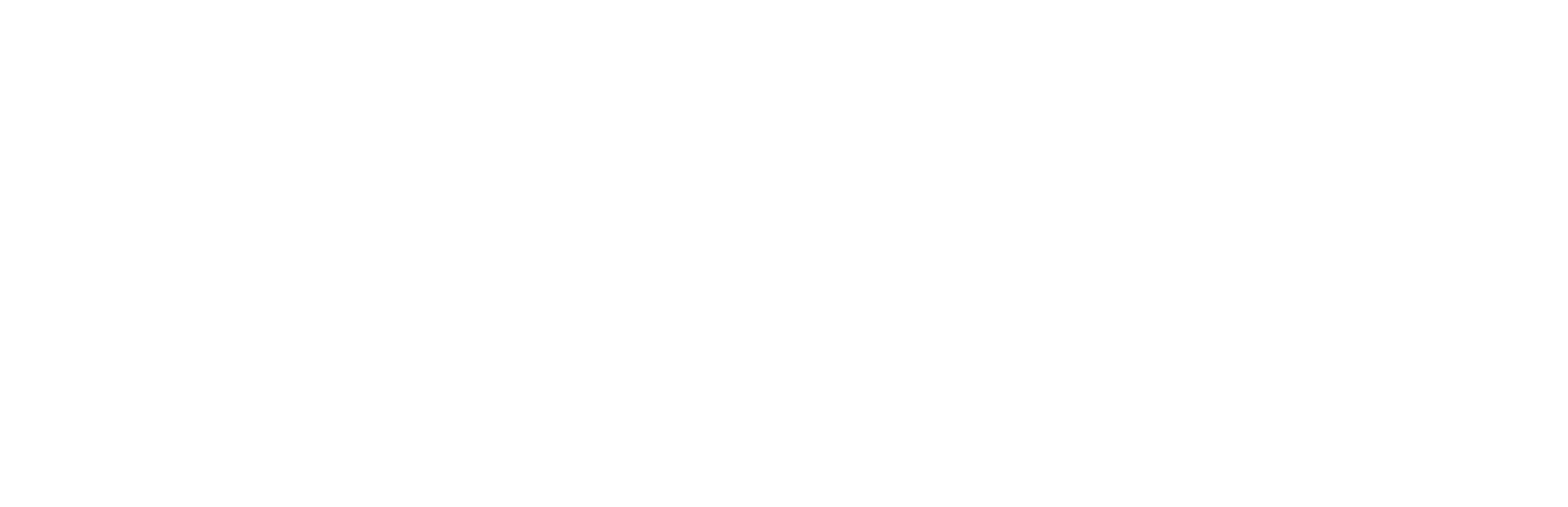
A 28-year-old male reported with 1-month history of painless dimness of vision in both eyes. He was a known high hyperopic since childhood, with no systemic illness. His best corrected visual acuity in the right eye (RE): 6/24, N:18 (+14.00DS/−1.50DC × 90°) and left eye (LE) was 6/18, N:12 (+12.50DS/−0.75DC × 90°). On slit lamp biomicroscopy, anterior segment findings were normal in both eyes. Corneal diameter was 10.5 mm, anterior chamber was slightly shallow in both eyes clinically and lens thickness appeared normal. Intraocular pressure was within normal in both eyes. Fundus examination noted clear vitreous, disc was normal, gross macular detachment was noted in both eyes [Figure 1a and b]. Fundus fluorescein angiography showed – mild hyperfluorescence in late film in both eyes [Figure 1c] RE and [Figure 1d] LE. On optical coherence tomography (OCT) – vitreoretinal interface was normal in both eyes with loss of foveal contour, overall increase in thickness of retina in both eyes, minimal intraretinal and gross subretinal fluid, was seen in both eyes in the form of hyporeflective areas in intraretinal and subretinal space. Increased choroidal thickness was seen in both eyes.
- (a) Pre-treatment fundus photo right eye, (b) pre-treatment fundus photo left eye, (c) pre-treatment fundus fluorescein angiography (FFA) right eye, (d) pre-treatment FFA left eye, (e) pre-treatment optical coherence tomography (OCT) right eye, (f) pre-treatment OCT left eye, (g) pre-treatment ultrasonography (USG) B-Scan right eye, and (h) pre-treatment USG B-Scan left eye. Bright Scan (B-Scan).
OCT showed macular detachment (819 nm) in RE [Figure 1e] and macular detachment of (812 nm) in LE [Figure 1f]. Ultrasonography Bright Scan ultrasonography (B-Scan) noted axial length of 17.1 mm in RE with hyperechoic dome shaped elevation of macular area [Figure 1g] and LE showed axial length of 16.8 mm with hyperechoic dome shaped mild elevation of macular area [Figure 1h]. Treatment options were discussed and informed consent was acquired from the patient. Patient received off-label intravitreal bevacizumab in both eyes. Under aseptic condition, 1.25 mg/0.05 mL of the drug was administered using 30-gauge needle through pars plana and the patient was followed up next day, at 1-week, 1-month, and then at monthly interval.
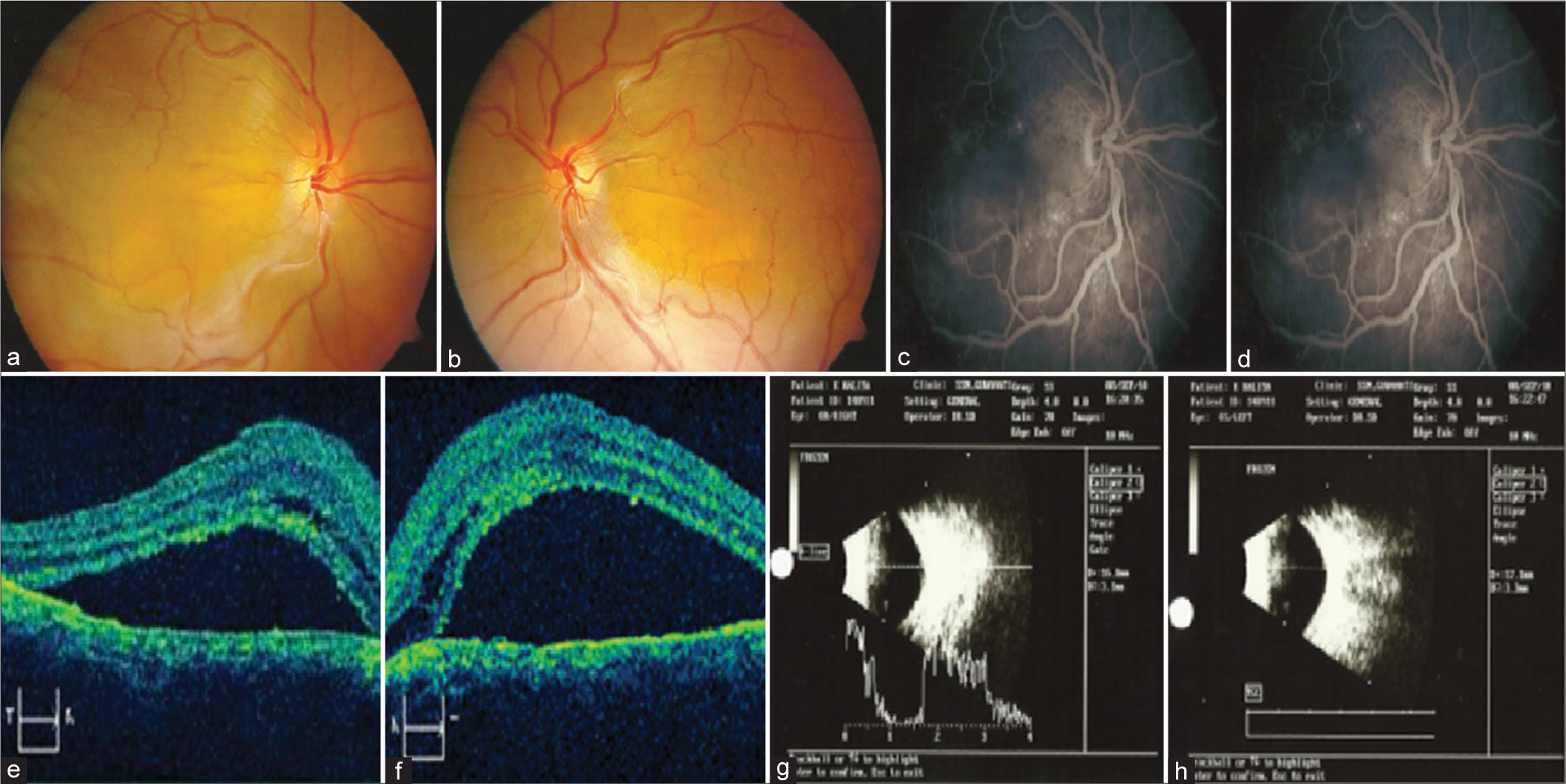
- (a) Post-treatment 1-month fundus photo right eye, (b) post-treatment 1-month fundus photo left eye, (c) post-treatment 1-month optical coherence tomography (OCT) right eye, and (d) post-treatment 1-month OCT left eye.
RESULTS
Figure 2a and 2b shows the fundus picture of RE and LE, respectively, after 1 month of treatment. Figure 2c and 2d shows the OCT image of RE and LE, respectively. Exudative retinal detachment (RD) resolved significantly at 1-month follow-up. Macular detachment reduced from 819 nm pre-treatment to 595 nm after 1-month post-treatment in RE and 812 nm to 493 nm in LE.
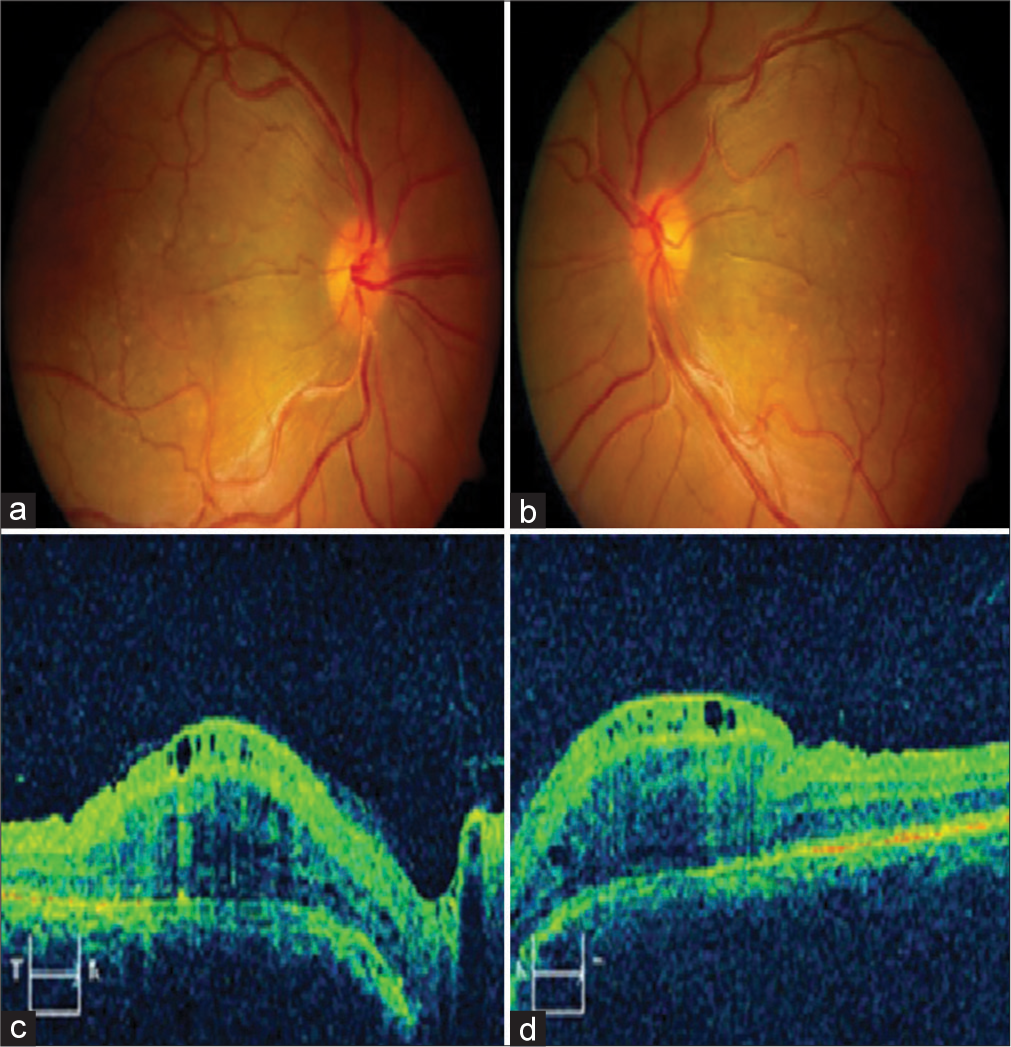
- (a) Post-treatment 2-month fundus photo right eye, (b) post-treatment 2-month fundus photo left eye, (c) post-treatment 2-month optical coherence tomography (OCT) right eye, and (d) post-treatment 2-month OCT left eye.
At 2-month post-treatment, fundus photo [Figure 3a] RE and [Figure 3b] LE, OCT image [Figure 3c], RE and [Figure 3d] LE showed partially resolved macular serous detachment necessitating repeat injection.
DISCUSSION
Nanophthalmos is a bilateral disease. Most commonly accepted hypothesis about etiopathogenesis of UES with nanophthalmos is abnormal scleral thickening, disorganized collagen fibers, leading to pressure over the vortex veins which cause congestion of choroidal veins and uveal effusion. Studies have shown that VEGF can counteract inflammation and reduce choroidal hyperpermeability.[7,8] Recent study showed that IL-6, IL-8, and VEGF levels in aqueous humor are increased in UES, showing that there might be some role of VEGF in the pathogenesis.[4-6] Surgical management of UES is with full or partial sclerotomies and vortex vein decompression.[9] In medical management, systemic and topical steroids were used in many studies with variable results. Guo et al. reported use of anti-VEGF agent for the treatment of intractable UES in patients who had partial sclerectomy, but effusion was poorly absorbed or relapsed.[8] They found VEGF, IL-6, and IL-8 levels in the aqueous humor of UES patients were elevated in all three cases. They reported the total resolution of suprachoroidal fluid and subretinal fluid in all three cases. Exact mechanism is unknown, but they hypothesized that anti-VEGF can decrease the activation of macrophages which results in decrease in IL-6 and IL-8 levels.
CONCLUSION
In our case, we decided to give Anti-VEGF alone. Significant resolution of exudative macular detachment was noted at 1-month follow-up and the patient required repeat injection at 2-month follow-up. Exact mechanism for fluid resorption is unknown but most probably it is related to decrease in inflammatory mediators that results in decrease in permeability of vessels, resulting in decrease in exudation. Hence, anti-VEGF is a safe and easy procedure in exudative macular detachment in nanophthalmic eyes instead of more invasive scleral resection. However, long-term follow-up, at least up to 12 months and further studies with more patients are required to establish the efficacy of this treatment modality.
Ethical approval
The author(s) declare that they have taken the ethical approval from IRB.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Satyen Deka is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Idiopathic serous detachment of the choroid, ciliary body, and retina (uveal effusion syndrome) Ophthalmology. 1982;89:1018-32.
- [CrossRef] [PubMed] [Google Scholar]
- Nanophthalmos with uveal effusion. A new clinical entity. Arch Ophthalmol. 1975;93:1989-99.
- [CrossRef] [PubMed] [Google Scholar]
- The pathogenesis and treatment of complications in nanophthalmos. J Ophthalmol. 2020;2020:6578750.
- [CrossRef] [PubMed] [Google Scholar]
- Intravitreal anti-VEGF therapy blocks inflammatory cell infiltration and re-entry into the circulation in retinal angiogenesis. Invest Ophthalmol Vis Sci. 2012;53:4323-8.
- [CrossRef] [PubMed] [Google Scholar]
- Early effects of dexamethasone and anti-VEGF therapy in an inflammatory corneal neovascularization model. Exp Eye Res. 2014;125:118-27.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular endothelial growth factor (VEGF)-key factor in normal and pathological angiogenesis. Rom J Morphol Embryol. 2018;59:455-67.
- [Google Scholar]
- The vascular endothelial growth factor (VEGF)/VEGF receptor system and its role under physiological and pathological conditions. Clin Sci (Lond). 2005;109:227-41.
- [CrossRef] [PubMed] [Google Scholar]
- Partial thickness sclerectomy and intravitreal anti-VEGF therapy for intractable uveal effusion syndrome. Int Ophthalmol. 2019;39:1885-90.
- [CrossRef] [PubMed] [Google Scholar]
- Full-thickness sclerotomy for uveal effusion syndrome. Korean J Ophthalmol. 2013;27:294-8.
- [CrossRef] [PubMed] [Google Scholar]