Translate this page into:
Acquired vitelliform lesion: A lesser diagnosed entity

*Corresponding author: Jaydeep Avinash Walinjkar, Department of Vitreo-Retina, Aditya Jyot Eye Hospital (A Unit of Dr Agarwal’s Eye Hospital), Mumbai, Maharashtra, India. drjaydeep23@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Walinjkar JA, Patel AQ, Sundaram SN. Acquired vitelliform lesion: A lesser diagnosed entity. J Ophthalmic Res Pract. 2024;2:35-7. doi: 10.25259/JORP_43_2023
Abstract
We report a case of 56-year-old female patient who came to our retina department with diminution of vision in both eyes (BE) for three years. She was treated with anti-vascular growth factor injections in BE for choroidal neovascular membrane (CNVM) at another medical facility three months back. Her best corrected visual acuity (BCVA) was 6/24, N18, and 6/9, N8 in the right and left eyes, respectively. Fundus showed vitelliform lesions and subretinal deposits in BE. We could not find any evidence of CNVM on optical coherence tomography (OCT) angiography. We made a provisional diagnosis of adult-onset foveomacular dystrophy (AOFVD). After the literature review and investigations, we made a clinical diagnosis of acquired vitelliform lesion (AVL). The lesion is usually located between the retinal pigment epithelium and photoreceptors, which may occur as an isolated entity or in conjunction with other comorbidities. Hence, it is very important to differentiate AVL from CNVM to avoid unnecessary treatment.
Keywords
Acquired vitelliform lesion
Adult-onset vitelliform dystrophy
Choroidal neovascular membrane
Misdiagnosis
Macular atrophy
INTRODUCTION
Acquired vitelliform lesion (AVL) is a rarely diagnosed entity and often misdiagnosed as adult-onset vitelliform dystrophy (AOFVD) or choroidal neovascular membrane (CNV). AVL usually shows up in older adults and is linked to age-related changes[1] On the flip side, AOFVD is a genetic condition that tends to be hereditary which shows up in adulthood with similar clinical features like yellowish deposit at the macula. However, it is caused by specific genetic mutations when it comes to the impact on vision, both AVL and AOFVD can cause central vision distortion or blurriness.[2] However, the progression and severity of vision changes can differ between the two conditions. AVL can be differentiated from CNV with the help of fundus fluorescein angiography or non invasive OCT-angiography techniques.[2,3]
CASE REPORT
A 56-year-old female presented to us with reduced vision in both eyes (BE) for three years. Right eye (RE) best corrected visual acuity (BCVA) was 6/24, N18, and left eye (LE) was 6/9, N8. She gave a history of choroidal neovascular membrane (CNVM) for which she received an intravitreal injection of bevacizumab in BE three months back at a different medical facility. BE anterior segment was unremarkable. The posterior segment showed a subfoveal scar in the RE, a yellowish lesion at the center of the macula in the LE, and bilateral subretinal drusenoid deposits (SRDDs) [Figures 1a and b]. CIRRUS™ high-definition optical coherence tomography (HD-OCT) (model 5000, Carl Zeiss Meditec, Inc., Dublin, CA) of the RE demonstrated a subfoveal hyper-reflective material and loss of ellipsoid zone [Figure 1c]. LE revealed a hyporeflective lesion subfoveal and thickened ellipsoid zone [Figure 1d]. Angioplex™ OCT angiographic imaging on the CIRRUS™ HDOCT showed no evidence of CNVM in either eye [Figure 2a and b]. The lesion was misdiagnosed as CNVM previously, and the patient was intervened needlessly. In cases where the patient is not keen for fundus fluorescein angiography, which is an invasive method, optical coherence tomography angiography (OCTA) can be performed to detect vascular abnormality.
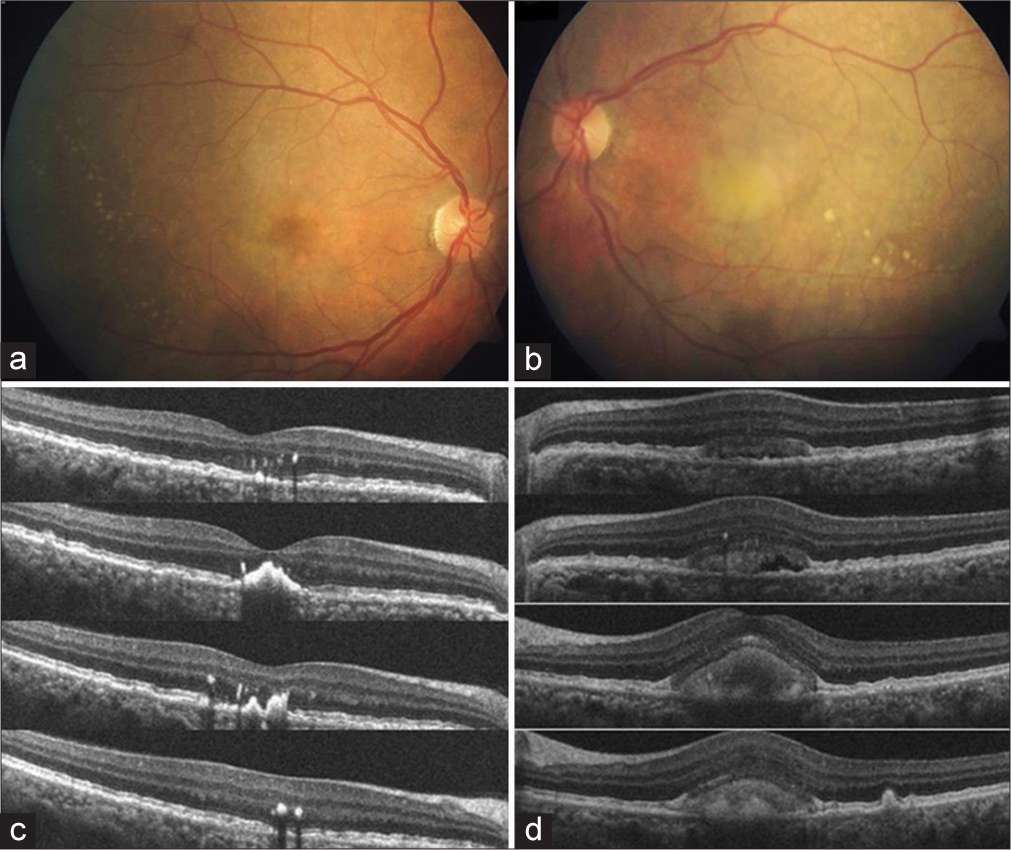
- (a) Showing subfoveal scar and subretinal drusenoid deposits. (b) Showing classic egg-yolk lesion and subretinal drusenoid deposits. (c) Showing high-definition-optical coherence tomography (HDOCT) scans of the right eye with subfoveal hyper-reflective material with loss of ellipsoid zone. (d) Showing HD-OCT scans of the left eye with a subfoveal hypo-reflective material with ellipsoid zone and retinal pigment epithelium thickening.
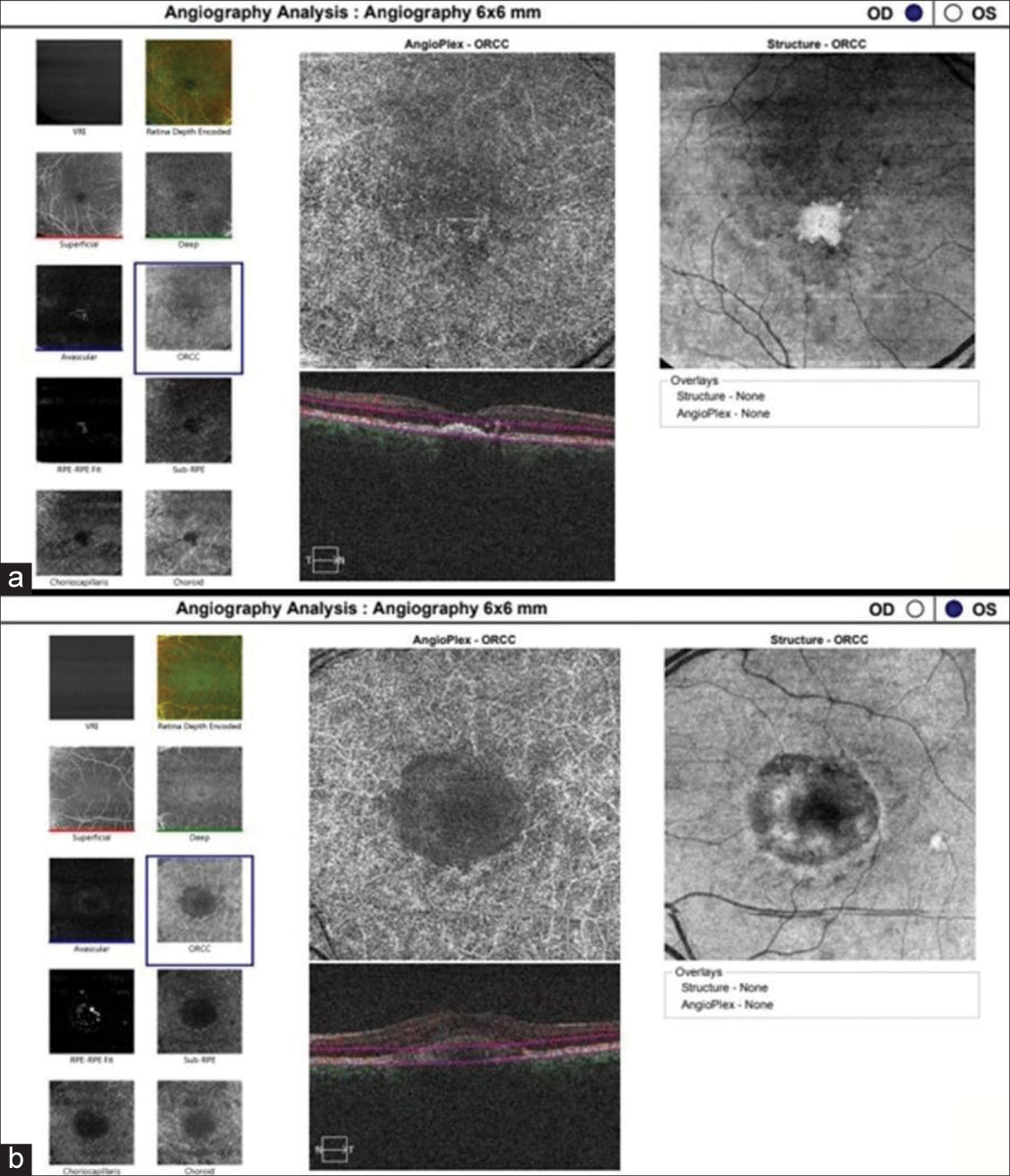
- (a) Optical coherence tomography angiography of outer retina to choriocapillaris zone of the right eye, (b) left eye demonstrating no evidence of any vascular network or other vascular abnormality. OD: oculus dexter (right eye), OS: oculus sinister (left eye), ORCC: outer retina to choriocapillaris.
EOG was performed, and BE results were subnormal. Based on the clinical examination and investigations, we made a diagnosis of adult-onset foveomacular dystrophy (AOFVD). However, in the absence of a family history of genetic disorders and after the patient denied genetic testing, we termed it an acquired vitelliform lesion (AVL) that occurs in the fourth and fifth decades of life.[1] The presence of SRDD in BE and the early atrophic stage in the RE also led to the diagnosis of AVL.
DISCUSSION
Yellowish or pigmented subretinal lesions may occur in a wide range of retinal disorders.[2] Few common associations of AVL are early age-related macular degeneration, cuticular drusen, tractional maculopathies, and SRDD.[3] Risks of the development of macular atrophy, CNVM, and macular holes have been reported in the case of AVL.[3,4] Lesion progresses to the atrophic stage faster in AVL than in AOFVD.[5] Patients with AVLs should be assessed regularly for early detection of possible complications. However, the lesion should not be confused with CNVM to avert needless interventions.
CONCLUSION
In summary, understanding the difference between AVL and AOFVD is crucial to differentiate the disease and make correct diagnosis. Whether age-related or genetic, both conditions impact the macula in distinct ways. It is also important to avoid improper and unnecessary treatment.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Macular disease resembling adult foveomacular vitelliform dystrophy in older adults. Ophthalmology. 1987;94:362-6.
- [CrossRef] [PubMed] [Google Scholar]
- Advanced imageJ analysis in degenerative acquired vitelliform lesions using techniques based on optical coherence tomography. Biomedicines. 2023;11:1382.
- [CrossRef] [PubMed] [Google Scholar]
- Natural course of adult-onset vitelliform lesions in eyes with and without comorbid subretinal drusenoid deposits. Int Ophthalmol. 2020;40:1501-8.
- [CrossRef] [PubMed] [Google Scholar]
- Progression of an acquired vitelliform lesion to a full-thickness macular hole documented by eye-tracked spectral-domain optical coherence tomography. Arch Ophthalmol. 2012;130:1221-3.
- [CrossRef] [PubMed] [Google Scholar]
- Multimodal image analysis in acquired vitelliform lesions and adult-onset foveomacular vitelliform dystrophy. J Ophthalmol. 2016;2016:6037537.
- [CrossRef] [PubMed] [Google Scholar]