Translate this page into:
Topical 5-fluorouracil as monotherapy for ocular surface squamous neoplasia

*Corresponding author: Francis Ezra Miciano Laxamana, Department of Ophthalmology, Eye and Vision Institute, The Medical City, Pasig City, Philippines boz_lax@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Laxamana FM, Mercado GV. Topical 5-fluorouracil as monotherapy for ocular surface squamous neoplasia. J Ophthalmic Res Pract. 2024;2:84-9. doi: 10.25259/JORP_23_2024
Abstract
Ocular surface squamous neoplasia (OSSN) comprises a gamut of diseases, which encompass conjunctival intraepithelial neoplasia, conjunctival carcinoma in situ, and squamous cell conjunctival neoplasia. Gold standard treatment for OSSN entails excision with cryotherapy. A lot of progress has been made recently that shows that chemotherapeutic drugs, such as mitomycin C, 5-fluorouracil (5-FU), and interferon alfa2b, can be just as effective. This is a case report that includes two cases: An 81-year-old Filipino female and a 65-year-old Filipino male who presented with a pinkish lesion on the bulbar conjunctiva. Documentation was done through clinical observation, slit-lamp examination, and the use of anterior segment optical coherence tomography (OCT). 1% topical 5-FU was given as chemotherapy administered at 1 drop 4×/day for 1 week with a 3-week drug holiday. During the course of treatment, we noted clinical resolution of the lesions grossly on slit-lamp examination. On anterior segment OCT, a decrease in diameter and thickness was noted, but with remaining areas of hyperreflectivity and thickened epithelium at the site of the lesion. No decrease in visual acuity was noted during the course of treatment, as well as any adverse effects such as eye pain or inflammation. Considering its safety and efficacy profile, 5-FU has great potential to be considered as a first-line therapy in the topical treatment of OSSN. Topical chemotherapy can target microscopic diseases that may be missed surgically and decrease adverse effects. As seen in this case report, 5-FU shows much promise as a possible alternative in the treatment of OSSN.
Keywords
Ocular surface squamous neoplasia
5-fluorouracil
Topical chemotherapy
Anterior segment optical coherence tomography
Squamous cell conjunctival neoplasia
INTRODUCTION
Ocular surface squamous neoplasia (OSSN) comprises a gamut of epithelial squamous malignancies ranging from dysplasia to invasive carcinoma.[1] Prior history of OSSN, exposure to ultraviolet (UV) light, previous skin cancer, advanced age, and male gender are risk factors for OSSN.[2] OSSN is thought to arise from dysfunctional limbal stem cells that have been altered by mutagenic agents such as UV radiation. UV rays cause DNA damage by inducing p53 gene mutations, which have been reported in individuals with OSSN. The etiology of OSSN is multifaceted. Viruses which are known to be associated with OSSN are human papillomavirus, Hepatitis B and C, and human immunodeficiency 1 and 2 viruses. Environmental factors involved are chronic cigarette smoking, use of petroleum products, and chemicals such as arsenic and beryllium.[3]
OSSN lesions clinically have a papillary, gelatinous, leukoplakic, or opalescent appearance. They may be raised or flat, diffuse or localized, and may have a feeder conjunctival vessel. Limbal stem cells are typically implicated for causing OSSN. Sufficiently thick tumors are limited within the epithelium, although massive tumors can infiltrate deeper corneal stroma. It is locally invasive and can invade intraocular tissues and orbit.[4] Tumor borders can be determined well by vital dye staining with toluidine blue, rose bengal, or lissamine green.[5] Tissue sampling is done with fine-needle aspiration biopsy, exfoliative cytology, or impression cytology.[5] High-resolution segment optical coherence tomography (HR-OCT), fluorescent microscopy, and confocal microscopy are the imaging tools to help in diagnosis.
The gold standard in OSSN management consists of surgical excision with cryotherapy, which has both therapeutic and diagnostic potential.[6] However, surgery has certain drawbacks, including conjunctival scarring, limbal stem cell deficiency, and/or leaving residual disease, which can be a cause of recurrence.[5] Microscopic subclinical residual diseases are responsible for the reported recurrence rates of 33% with negative surgical margins and up to 56% when margins are positive.[6] Medical treatment for OSSN has gained popularity as it can do away with risk and does not necessitate treating the whole ocular surface.
Chemotherapeutic agents used for the treatment of OSSN include interferon-alpha-2b, mitomycin-C, and 5-fluorouracil (5FU).[7] 5-FU is a pyrimidine analog which blocks the enzyme responsible for DNA base thymidine synthesis. Topical 5-FU can attain clinical resolution in 85% of cases, with the possibility of recurrence being 12.5–43%.[4] According to a retrospective, interventional case series study by Venkateswaran et al., 96.3% of lesions treated with 5-FU resolved completely (median number of cycles was 4, with a mean treatment of 6.6 months, n = 52 eyes).[2]
In the Philippines, OSSN accounts for 40.4% of all malignant conjunctival tumors, followed by its precursor, conjunctival intraepithelial neoplasia (CIN), with 26.3%.[8] The rapid popularity of non-invasive treatments such as topical chemotherapeutic agents should be given importance since this can be beneficial to developing countries with limited medical resources.
CASE REPORTS
Case 1
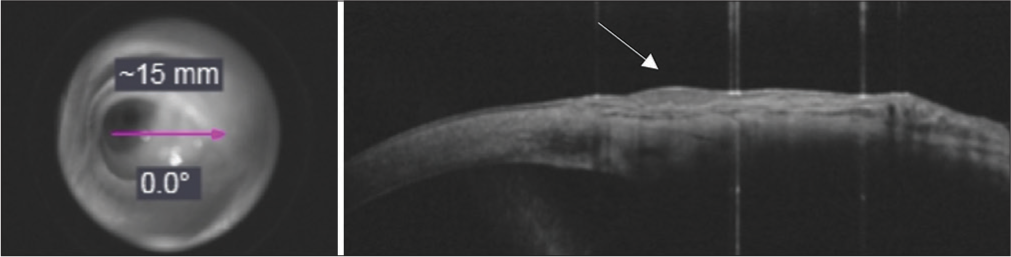
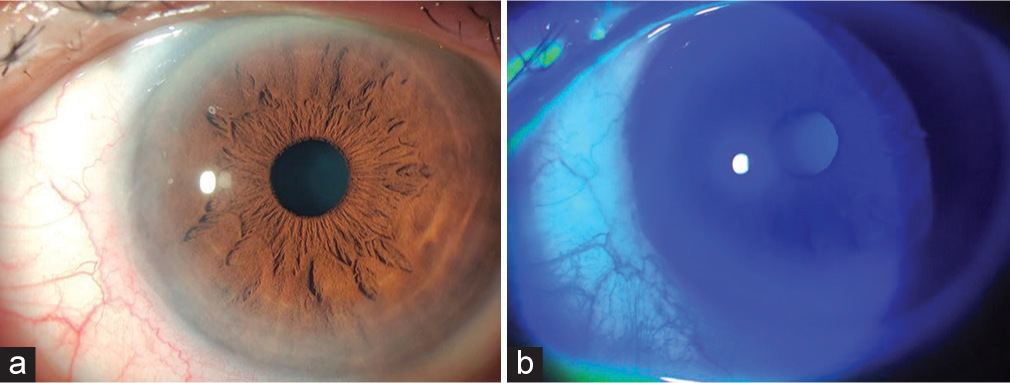
An 81-year-old Filipino woman reported a 2-month history of a fleshy mass on the right eye that was noted to be gradually increasing in size. This was accompanied by pruritus and occasional foreign body sensation. On examination, the best-corrected visual acuity was 20/40 on the right eye and 20/50 on the left eye. Slit-lamp biomicroscopy showed a 5.5 × 8 mm fleshy mass with distinct borders encroaching the limbus at the inferonasal portion around 4–5 clock hours (h) of the bulbar conjunctiva of the right eye. There were multiple feeder vessels noted nasal to the lesion as well [Figure 1a]. On staining with fluorescein dye, there were areas of multiple pinpoint superficial punctate dye uptake inferiorly and adjacent to the lesion. In addition, the lesion showed uptake of the fluorescein dye, and lissamine green, which stains devitalized ocular surface epithelial cells, showed dye uptake beyond the gross border [Figure 1b]. The fundus examination was unremarkable. Anterior segment OCT was done, which showed a hyperreflective, thickened epithelium with an abrupt transition from normal to abnormal epithelium exhibiting posterior shadowing [Figure 2].

- Before initiation of 5-fluorouracil treatment (a) Slit-lamp examination showed a 8 × 5.5 mm pinkish fleshy lesion with distinct borders and feeder vessels, encroaching the limbus, (b) lesion stained with Lissamine green.

- Before initiation of 5-fluorouracil treatment, en face projection of OCT signal from cornea to conjunctiva (pink arrow). Anterior segment optical coherence tomography (OCT) of lesion showing a zone of hyperreflectivity and thickened epithelium corresponding to the conjunctival lesion (white arrow).
Due to the clinical presentation and the possible risk factor of sun exposure, we decided to treat the patient as a case of OSSN (CIN vs. squamous cell carcinoma). Initially, we opted to excise the lesion with the use of the no-touch surgical technique, with alcohol epitheliectomy, and cryotherapy of the margins. However, due to the situation at the time being at the height of the COVID-19 lockdown and considering the patient’s age and risk, conservative options such as topical chemotherapy were considered.
Due to logistical and technical constraints, as well as a delay in the procurement of the drug, the patient followed up after 1 month to start treatment. On examination, the lesion increased in size to 9 × 6.5 mm. A 5-FU stock preparation of 500 mg/10 mL was diluted by mixing 2 mL with 8 mL of normal saline solution. The final preparation of 1% 5-FU eye drops was administered at 1 drop 4 times a day for 1 week, followed by a 3-week drug holiday, which is equivalent to 1 cycle. To address the adverse effects such as irritation and discomfort, sodium hyaluronate eye drops were used as lubricant and applied 1 h after administration of 5-FU. Based on the available literature, there are no practice patterns given for the choice of lubricant eyedrops in topical chemotherapy for OSSN. The choice of supplement lubricant was based on preference and availability.
The patient followed up after 2 weeks with a noted reduction in lesion size after the completion of 1 week of continuous treatment. No pain or eye discomfort was noted at this time. On examination, the lesion was measured to be 7 × 5.5 mm, with minimal whitish discharge noted at the periphery of the lesion temporally [ Figure 3a]. There was uptake of fluorescein dye by the lesion [Figure 3b].

- After 2 weeks of treatment of topical 5-fluorouracil, (a) Decrease in size of lesion noted. (b) Uptake on the lesion with fluorescein dye.
On the next follow-up, the patient had completed the 3rd week of the drug holiday, ending the first cycle of treatment. At the start of the second cycle of 5-FU, the lesion could not be visualized grossly, but the feeder vessels were still noted to be present [Figure 4a]. On staining with fluorescein dye, pinpoint uptake was noted at the lesion site [ Figure 4b]. Anterior segment OCT was done, and a hyperreflective area with thickening of the epithelium was still observed, but with a significant decrease in thickness as compared to the previous imaging [Figure 5].

- After completion of 1 cycle of treatment, (a) Noted a gelatinous lesion with feeder vessels encroaching limbus. (b) Punctate staining of the lesion with fluorescein dye.
- After completion of 1 cycle of treatment, en face projection of OCT signal from cornea to conjunctiva (pink arrow). Anterior segment optical coherence tomography (OCT) of lesion showing a decreased zone of hyperreflectivity (white arrow).
At the completion of the second cycle of treatment, the lesion was not visible clinically but still had tortuous vessels on the conjunctiva [ Figure 6a]. There was minimal punctate staining of the lesion with fluorescein dye [Figure 6b]. Repeat OCT of the area of the lesion showed a further decrease in the zone of hyperreflectivity and thickening [Figure 7]. After completion of three cycles of treatment, no gross lesion was seen, but feeder vessels were still visible [Figure 8a]. Minimal punctate staining of the lesion with fluorescein dye was seen [Figure 8b]. Anterior segment optical coherence tomography (OCT) of lesion still showed a zone of hyperreflectivity on the conjunctiva [Figure 9].

- After completion of 2 cycles of treatment, (a) No gross lesion seen but still with feeder vessels. (b) Minimal punctate staining of the lesion with fluorescein dye.

- After completion of two cycles of treatment, en face projection of OCT signal from cornea to conjunctiva (pink arrow). Anterior segment optical coherence tomography (OCT) of lesion showing a decreased zone of hyperreflectivity on the conjunctiva (white arrow).
- After completion of three cycles of treatment, (a) No gross lesion seen but still with feeder vessels. (b) Minimal punctate staining of the lesion with fluorescein dye.

- After completion of three cycle of treatment, en face projection of OCT signal from cornea to conjunctiva (pink arrow). Anterior segment optical coherence tomography (OCT) of lesion still showing a zone of hyperreflectivity on the conjunctiva (white arrow).
Case 2
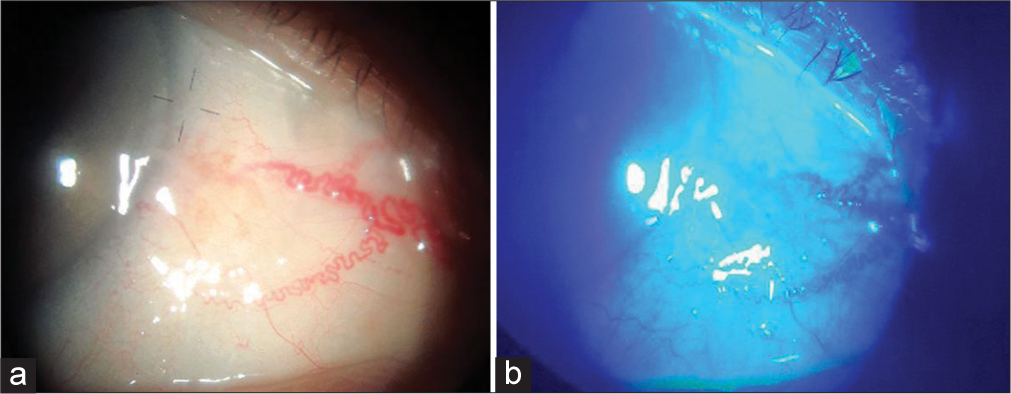
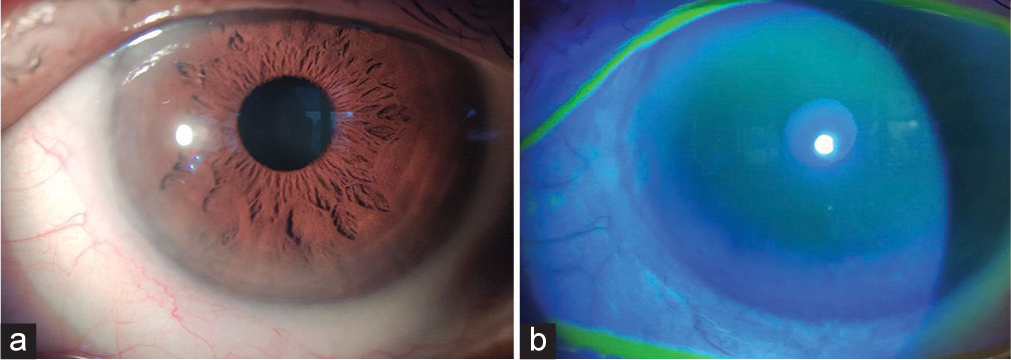
A 65-year-old Filipino male came in due to a red eye with a foreign body sensation on the left eye. No blurring of vision or eye pain was noted. On evaluation, the best-corrected visual acuity was 20/20 in both eyes. The conjunctiva of the left eye was hyperemic. Slit-lamp biomicroscopy of the left eye showed a fleshy mass on the nasal bulbar conjunctiva with indistinct borders. The lesion was encroaching on the limbus at the inferonasal portion and extended to the peripheral cornea at 10–5 o’clock. There are a few feeder vessels on the nasal aspect of the lesion [Figure 10a]. On staining with fluorescein dye, there was dye uptake on the cornea, revealing an epithelial lesion on the inferonasal peripheral cornea measuring 7 × 2 mm [Figure 10b]. Fundus examination was unremarkable. Anterior segment OCT showed a hyperreflective, thickened epithelium with an abrupt transition from normal and abnormal epithelium exhibiting posterior shadowing [Figure 11].
- Before initiation of 5-fluorouracil treatment (a) Slit lamp showed a fleshy mass on the nasal bulbar conjunctiva. (b) Dye uptake on cornea noted.

- Before initiation of 5-fluorouracil treatment, en face projection of OCT signal from conjunctiva to cornea (pink arrow). Anterior segment OCT showing an area of hyperreflectivity on the conjunctiva (white arrow) and thickened epithelium (blue arrow).
With our physical examination and clinical symptoms, supported by findings on the anterior segment OCT, the assessment at this time was OSSN. Due to the success of the first case, treatment with topical chemotherapy was started on the patient. 1% 5-FU eye drops were administered at 1 drop 4 times a day for 1 week, followed by a 3-week holiday. As with the first case, sodium hyaluronate eye drops were given as a lubricant to address the adverse effects of the chemotherapeutic drug. This was given 1 h after the administration of 5-FU.
The patient followed up after 2 weeks. There was still conjunctival hyperemia on the left. The patient felt mild discomfort on placing the eyedrops but was relieved with the administration of lubricants. On examination under the slit lamp, the lesion on the cornea was barely visible but still had areas of inferior dye uptake on staining with fluorescein [Figures 12a and b].

- After 2 weeks of treatment of topical 5-fluorouracil, (a) Lesion on the cornea barely visible. (b) Cornea still with areas of dye uptake inferiorly.
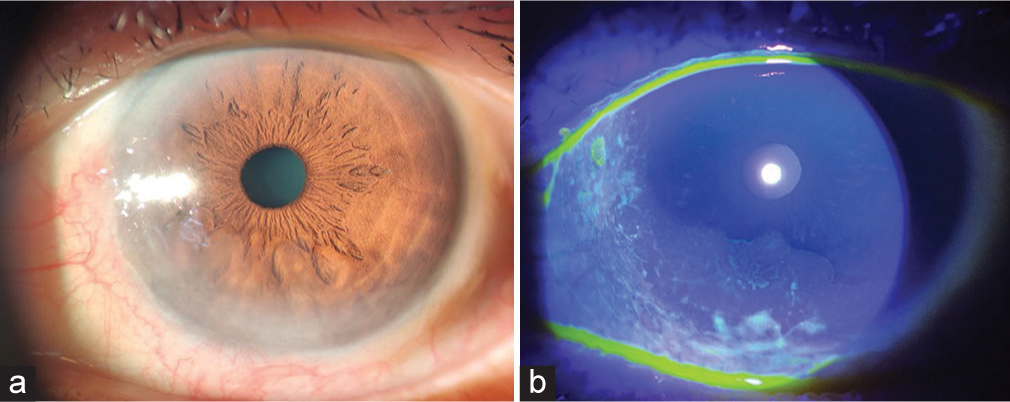
After completing the first cycle of treatment, the patient was seen with minimal conjunctival hyperemia. No subjective symptoms were noted in the left eye. On examination, no epithelial lesion was seen on the cornea, and there was no dye uptake with fluorescein [Figures 13a and b]. Anterior segment OCT showed a hyperreflective area with thickening of the epithelium but noted a decrease in size compared to the pre-treatment OCT with a smoother transition from normal to abnormal epithelium [Figure 14].

- After completion of 1 cycle of treatment. (a) lesion on the cornea barely visible on slit-lamp examination. (b) No epithelial lesion was seen on the cornea and no dye uptake with fluorescein.

- After completion of 1 cycle of treatment, en face projection of OCT signal from conjunctiva to cornea (pink arrow). Anterior segment OCT still with an area of hyperreflectivity on the conjunctiva (white arrow).
The patient followed up after completing the second cycle of treatment. Grossly, the lesion was not visible, and there was less conjunctival hyperemia in the left eye. There are still no subjective complaints, such as foreign body sensations or tearing. On examination, the cornea was clear, with no dye uptake on fluorescein staining [Figures 15a and b]. Anterior segment OCT still showed a decrease in hyperreflectivity but thickened epithelium [Figure 16].
- After completion of 2 cycles of treatment, (a) Clear cornea with no epithelial defect seen (b) no dye uptake on fluorescein staining.

- After completion of two cycles of treatment, en face projection of OCT signal from conjunctiva to cornea (pink arrow). Anterior segment OCT still with an area of minimal hyperreflectivity on the conjunctiva (white arrow).
After the completion of the third cycle of treatment, there was no conjunctival hyperemia seen in the left eye. There were still no subjective complaints, and the patient was compliant with the eye drops. On slit-lamp examination, no lesion was seen on the left eye, no epithelial defect and there was no dye uptake with fluorescein [Figures 17a and b]. Anterior segment OCT still showed an area of hyperreflectivity corresponding to the lesion [Figure 18].
- After completion of three cycles of treatment, (a) lesion on the cornea barely visible on slit-lamp examination. (b) No epithelial lesion was seen on the cornea and no dye uptake with fluorescein.

- After completion of three cycle of treatment, en face projection of OCT signal from conjunctiva to cornea (pink arrow). Anterior segment OCT still with an area of minimal hyperreflectivity on the conjunctiva (white arrow).
DISCUSSION
The first report of 5-FU in OSSN treatment came in 1986.[7] It is used as a topical 1% 5-FU in an aqueous solution. Studies have reported 5-FU as the primary treatment of OSSN, with a high resolution rate (average 91%, range 82–100%, n = 129). In several studies, 5-FU was used for 2–7 days, followed by a 30–45-day holiday (range of 1–6.5 cycles). Recurrences ranged from 0% to 28%, occurring in the 1st year. Common side effects encountered are ocular pain and lid inflammation.[2]
Parrozzani et al. reported 41 patients diagnosed with OSSN who were treated with 1% 5-FU as primary treatment. Twenty-three patients received a single 1% 5-FU course (56%), 15 cases (36%) received two courses, and three cases (7%) received three courses. Complete tumor regression was achieved in 34 cases (83%) after a mean of 1.5 courses (range, 1–3 courses). The mean time of tumor resolution was 11 ± 9 weeks (range, 3–22 weeks).[1] This strategy is characterized by one (30-day) or more courses followed by 1 month of no treatment between each course. Three patients (7.3%) developed an early recurrence.
In another study by Joag et al., 5-FU drops were given 4 times daily for 1 week, followed by a drug holiday for 3 weeks. This monthly cycle was continued till clinical resolution. Of the 44 eyes, 36 lesions (82%) were completely resolved with 5-FU therapy. Of these, the median number of cycles was 4.[7]
At present, HR-OCT imaging has been used to guide the length of treatment, which is thought to reduce the frequency of premature termination of medical therapy. The characteristic features of OSSN on OCT are as follows: (1) hyperreflective; (2) thickened epithelium; and (3) an abrupt transition point between normal and abnormal epithelium.[5] OCT being non-invasive, provides a definite edge in diagnosis, though it largely relies on the experience of the technician conducting the procedure.[5] OCT is used as a measure of treatment response. Clinically, lesions may appear resolved, but OCT determines subclinical disease that is not seen grossly with slit-lamp biomicroscopy. OCT has been an invaluable tool in the surveillance of treatment.
The two patients in this case report completed three cycles of 5-FU. As we observed, improvement was seen just 2 weeks after starting the medication. There were subjective symptoms in the second case, but they were addressed with the application of lubricant eye drops. On completion of the 2nd and 3rd cycles, there was gradual resolution of the lesion, which was noted on the anterior segment OCT.
CONCLUSION
5-FU, being used as a topical chemotherapeutic, should always be an option in the treatment of OSSN. Although it has been the mainstay of therapy and has the properties of being a diagnostic and therapeutic tool, surgical excision has its disadvantages, such as leaving microscopic residual disease, which can later on cause recurrence.
Topical chemotherapy has been gaining popularity for the past two decades, and an increasing number of studies are proving that it is indeed an acceptable option in the treatment of OSSN. In addition, anterior segment OCT is an important diagnostic procedure in its management as it monitors the response to therapy as well as detects any residual microscopic disease. It has been an invaluable tool in the patient’s follow-up as it is able to detect microscopic areas of disease not seen through slit-lamp biomicroscopy. In this case report, we have seen that the anterior segment OCT plays an important role in guiding the clinician with regard to deciding the number of cycles needed for the patient.
5-FU has had numerous reports showing its success as a monotherapy for OSSN. Given the clinical response of the patient and the OCT findings, it is indeed a promising choice for treatment. 5-FU can be considered as first-line treatment as per our observation but randomized control trials are required to establish this fact.
Acknowledgment
I would like to acknowledge and give my warmest thanks to my supervisor Dr. Gary Mercado and Dr. Patricia Tecson who made this work possible. Their guidance and advice carried me through all the stages of writing my project.
Ethical approval
The research/study approved by the Institutional Review Board at Institutional Review Board (IRB)- The Medical City Philippines, number N/A, dated March 15, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Topical 1% 5-fluoruracil as a sole treatment of corneoconjunctival ocular surface squamous neoplasia: Long-term study. Br J Ophthalmol. 2017;101:1094-9.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of topical 5-fluorouracil and interferon alfa-2b as primary treatment modalities for ocular surface squamous neoplasia. Am J Ophthalmol. 2019;199:216-22.
- [CrossRef] [PubMed] [Google Scholar]
- Ocular surface squamous neoplasia In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK573082 [Last accessed on 2024 Jun 22]
- [Google Scholar]
- Ocular surface squamous neoplasia-review of etio-pathogenesis and an update on clinico-pathological diagnosis. Saudi J Ophthalmol. 2013;27:177-86.
- [CrossRef] [PubMed] [Google Scholar]
- Update on pharmacotherapy for ocular surface squamous neoplasia. Eye Vis. 2019;6:24.
- [CrossRef] [PubMed] [Google Scholar]
- Management of ocular surface tumors: Excision vs. topical treatment. Vis Pan Am. 2014;13:86-9.
- [Google Scholar]
- Topical 5-fluorouracil 1% as primary treatment for ocular surface squamous neoplasia. Ophthalmology. 2016;123:1442-8.
- [CrossRef] [PubMed] [Google Scholar]
- Tumors of the eye and ocular adnexa at the Philippine Eye Research Institute: A 10-year review. Clin Ophthalmol. 2015;9:1239-47.
- [CrossRef] [PubMed] [Google Scholar]