Translate this page into:
Peripheral occlusive retinal vasculitis and associated hemi-central retinal vein occlusion in the same eye with suspected neuroretinitis: A rare case report

*Corresponding author: Jaydeep Avinash Walinjkar, Department of Vitreo-Retina, Aditya Jyot Eye Hospital (A unit of Dr. Agarwal’s Eye Hospital), Mumbai, India. drjaydeep23@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Walinjkar JA, Patel AQ, Sharma HR, Sundaram N. Peripheral occlusive retinal vasculitis and associated hemi-central retinal vein occlusion in the same eye with suspected neuroretinitis: A rare case report. J Ophthalmic Res Pract. 2024;2:28-31. doi: 10.25259/JORP_6_2024
Abstract
We describe a case of an 18-year-old male with decreased vision in the left eye (LE) over two weeks. At presentation, his uncorrected visual acuity was 6/6 in the right eye and light perception (PL+ve) in the LE. On ophthalmic examination, both eye’s anterior segments were unremarkable except a relative afferent pupillary defect in the LE. Posterior segment of the LE revealed peripheral active occlusive retinal vasculitis and hemi-central retinal vein occlusion superiorly along with suspected neuroretinitis. The diagnosis was confirmed with fundus fluorescein angiography and optical coherence tomography macula. He was not known to have any systemic illness previously and after relevant systemic investigations, he was treated empirically with intravenous methylprednisolone, oral steroids, anti-tubercular therapy, and anti-toxoplasma therapy. Retinal laser photocoagulation was done to the capillary non-perfusion areas. After three months from the day of presentation, visual acuity improved to 6/6 (partial), N6 in his LE.
Keywords
Retinal vasculitis
Vein occlusion
Optic disc edema
Macular star
INTRODUCTION
Occlusive retinal vasculitis (ORV) is characterized by an inflammatory ocular disease that can occur secondary to various systemic inflammatory disorders.[1] Ruling out the primary cause of the inflammation and treating it promptly is always recommended. Distinguishing between infectious and non-infectious causes of vasculitis is crucial to choose the correct line of treatment.[2] Active retinal vasculitis can sometimes occur in conjunction with retinal vein occlusion due to the blockage in the branch/tributary or central retinal vein that can abruptly cause diminution of vision.[3] It is a rare condition that may lead to potential visual loss if not diagnosed accurately and treated appropriately.
CASE REPORT
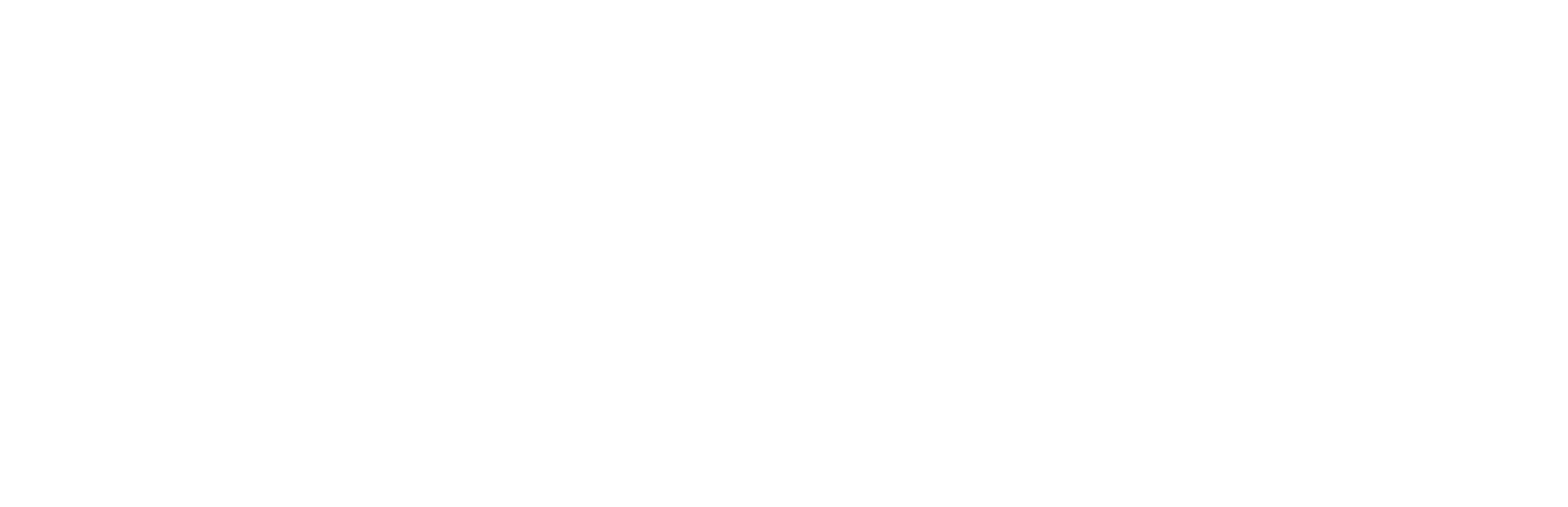
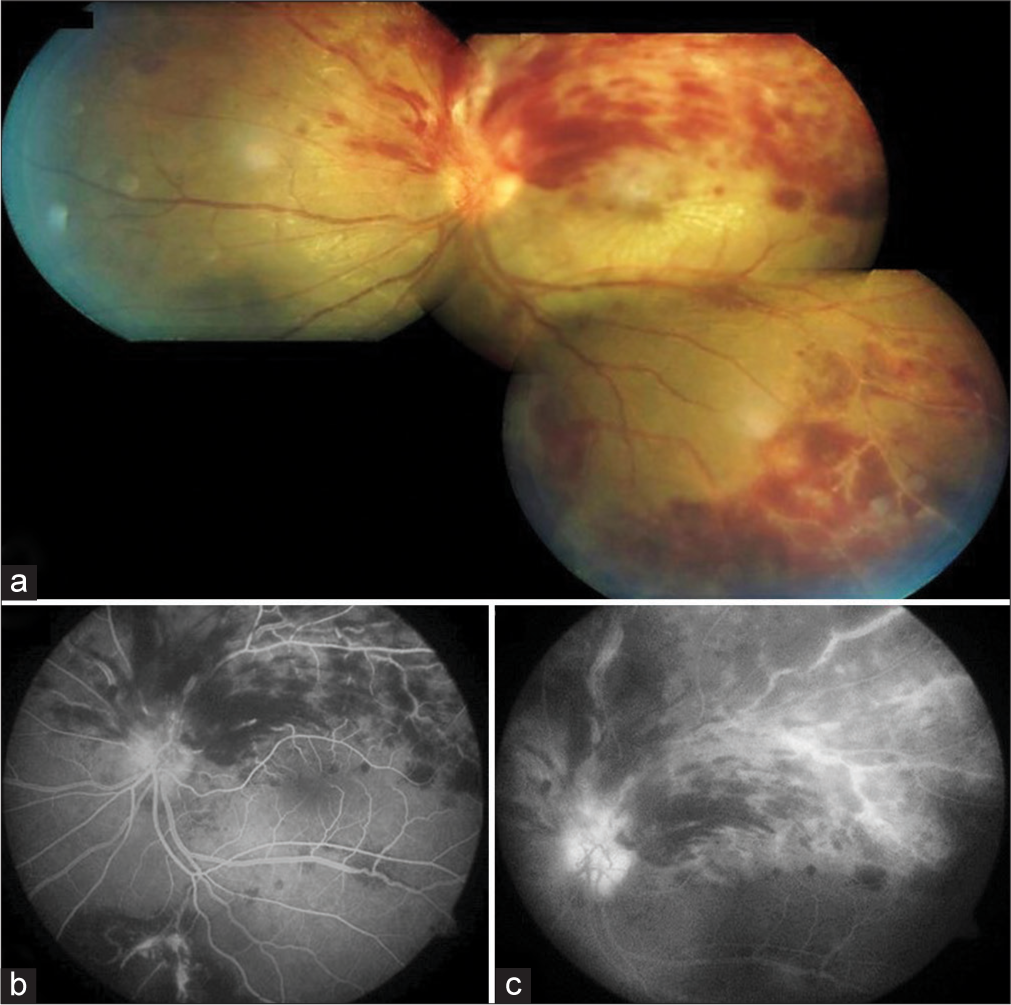
An 18-year-old male presented to us with progressive visual loss in the left eye (LE) for the past two weeks. No known systemic illness was presented. He had been diagnosed with suspected central retinal vein occlusion (CRVO) with macular edema at some other ophthalmic facility and advised anti-vascular endothelial growth factor (VEGF) therapy. He had come to us for a second opinion. On examination, the uncorrected visual acuity (UCVA) was 6/6, N6, and PL+ve in the right and LEs, respectively. The swinging flashlight test confirmed the presence of a positive relative afferent pathway defect in the LE. Slit-lamp examination of BE showed no evidence of anterior segment inflammation. Fundus examination with an indirect ophthalmoscope revealed optic disc edema, splinter hemorrhages superiorly, peripheral ORV with perivascular cuffing inferiorly, and a partial macular star in the LE [Figure 1a]. Optical coherence tomography, which was done elsewhere of poor signal strength, demonstrated cystoid macular edema (CME) and sub-foveal neurosensory detachment. A clinical diagnosis of active ORV and hemi-retinal vein occlusion (CRVO) was made with suspected neuroretinitis in the LE. Standard systemic investigations for ORV and CRVO were advised such as complete blood count (hemogram), erythrocyte sedimentation rate (ESR), random blood sugar, hemoglobin A1C, lipid profile, coagulation profile, serum homocysteine, serum angiotensin-converting enzyme (ACE), carotid Doppler, and 2D echo, to rule out the cause and confirm the diagnosis along with intravenous methylprednisolone (IV MP) for three days under the physician’s care. After three days, he was instructed to take IV MP (1 g) in 100 mL for two more days. IV MP was given as a rescue therapy in view of light perception vision, extensive ORV, and optic disc edema. All the systemic investigations were found within normal limits except for toxoplasmosis Immunoglobulin (Ig) G, cytomegalovirus IgG, and Mantoux. We had ruled out all common rheumatological conditions by appropriate investigations (Rheumatoid arthritis factor, anti-cyclic citrullinated peptide, anti-nuclear antibody, C-reactive protein, and ESR), which led to treating the patient empirically in a desperate attempt to salvage some vision in the affected eye. He was started on oral steroids, anti-tuberculosis therapy (ATT), topicals (prednisolone in tapering dose for 6 weeks), sulfamethoxazole (800 mg), and trimethoprim (160 mg) as the systemic investigations showed strongly positive Mantoux and toxoplasma IgG test as the affected eyes vision had only marginally improved after five doses of IV MP. He was started on ATT after appropriate consultation with a chest physician who recommended starting it empirically, as tuberculosis is one of the common etiologies for ORV.[4] A tapering course of oral steroids was given in accordance with standard treatment protocol for ORV of presumed tuberculous origin (Eales disease).[5] In view of a potentially blinding condition in a young adult, systemic treatment was continued further as the patient showed visual improvement subsequently (anti-toxoplasmosis treatment was stopped after its standard course). After 10 days from the initial presentation, fundus fluorescein angiography (FFA) was performed [Figure 1b and c]. LE showed extensive blocked fluorescence due to multiple retinal hemorrhages and acute superior hemi CRVO picture. Disc collateral was seen with late-phase disc staining. No CME was seen in the late phase. Suspected neovascularization elsewhere noted in inferotemporal quadrant at the border of the normal retina and retinal hemorrhages with capillary nonperfusion (CNP) areas. In view of the active condition, the laser photocoagulation was deferred for some time. After 3 months, the UCVA improved to 6/6 partial, N6 with significantly resolved hemorrhages, vasculitis, hard exudates, and optic disc edema. FFA-guided retinal photocoagulation was done to the CNP areas in the superior half and inferior periphery of the retina in three sessions. Post 1 month, both eyes fundi were found stable with laser marks [Figure 2a and b].
- (a) Montage image showing multiple splinter hemorrhages superiorly and occlusive retinal vasculitis inferiorly with partial macular star exudation (b) and (c) after 5 days of intravenous methylprednisolone, fundus fluorescein angiography showing blocked fluorescence corresponding to the retinal hemorrhages. No macular edema was seen.
- (a) Showing no cystoid macular edema. (b) Significantly resolved hemorrhages and exudates are seen with laser photocoagulation scars.
DISCUSSION
ORV can be present as a sight-threatening complication in young adults with various other ocular entities.[1] It refers to inflammation and blockage of the blood vessels or arteries in the retina. This can result in reduced blood flow and oxygen supply to the affected area, leading to vision impairment in the influenced eye.[2] ORV can be associated with other comorbidities such as vein occlusion and neuroretinitis.[3] In some cases, the inflammation and blockage of the retinal blood vessels caused by retinal vasculitis can lead to the development of hemi-central retinal vein occlusion.[4] Both entities are seen to be affecting the similar quadrant of the retina in most of the reported cases.[4] Unlike, in our case, retinal vasculitis was seen inferiorly and vein occlusion occurred in the superior half of the retina which may have caused the profound drop in vision of the affected eye. The authors of a study involving 30 patients discovered that a combination of aggressive treatment methods, such as systemic steroids, ATT, full panretinal photocoagulation, and early vitrectomy when needed, can give favorable anatomical and visual outcomes for individuals with Eales disease.[5]
In a study conducted by Yoshizawa et al. they presented a case of 16-year-old male who presented with sudden loss of vision and idiopathic severe inflammatory manifestation, including CRVO, disc, and macular edema with a macular star.[6] He was immediately started on oral prednisolone 30 mg/d with a tapering dose. After one week, macular edema was reduced and vision improved from 0.04 to 1.0. At 4 months follow-up, vision dropped to 0.01 and marked macular edema with peripheral vasculitis was seen. He was then treated with IV MP for three days, along with oral prednisolone and prophylactic laser photocoagulation to the CNP areas. At the final visit, his visual acuity improved to 0.1.[6] The treatment followed in this case after the recurrence of macular edema was indistinguishable from our case. Another similar retinal presentation was seen in a 47-year-old patient with Crohn’s disease (inflammatory disease), she was treated well with immunosuppressive therapy, oral steroids, and anti-VEGF therapy (for macular edema). Complete resolution of CRVO and retinal vasculitis was achieved after 1 year with 10/10 visual acuity.[7] Although, in our case, macular edema resolved following five doses of IV MP which was primarily administered for the suspected neuroretinitis. Ooi et al., in 2011, reported a case of combined central retinal artery occlusion and optic neuropathy with retinal vasculitis in a young male with presumed tuberculous etiology. They treated the patient well with ATT, antibiotics, and retinal laser photocoagulation to the CNP areas but no visual recovery was obtained.[8] Our patient responded well to ATT. The potential visual recovery gained in our case was probably due to the active IV MP treatment for optic disc edema which may have worked for reducing the macular edema as well, as noted on the FFA which was performed after five doses of IV MP. Although to the best of our knowledge, there is no literature available to support the mechanism of action of IV MP for macular edema. Some studies and case series have revealed that the high dose intravenous steroid therapy can significantly and/or completely improve the disc edema and restore potential visual acuity.[9,10] In summary, cases with no significant systemic or active manifestation of tuberculosis or other sporadic inflammatory conditions can make the diagnosis difficult. A strong suspicion is required to reach an accurate diagnosis. However, sometimes in the absence of an accurate diagnosis, emergent empirical treatment can be considered as a rescue therapy in a potentially blinding condition. The treatment regimen followed in our case can be considered to achieve good results by rapidly controlling active inflammation. In this kind of case, misdiagnosis can lead to the wrong treatment choice or delayed treatment, which may cause disastrous and irreversible visual loss.
CONCLUSION
Timely diagnosis and appropriate treatment can avert sight-threatening complications and sometimes miraculously restore the vision in such devastating conditions. To the best of our knowledge, this is the first case report demonstrating the unusual presentation of active ORV with hemi-central vein occlusion in the same eye in a young patient.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Unusual presentation of ocular tuberculosis: Multiple chorioretinitis, retinal vasculitis and ischaemic central retinal vein occlusion. Clin Exp Optom. 2013;96:428-9.
- [CrossRef] [PubMed] [Google Scholar]
- Ocular vasculitis: A multidisciplinary approach. Curr Opin Rheumatol. 2005;17:25-33.
- [CrossRef] [PubMed] [Google Scholar]
- Differential diagnosis of retinal vasculitis. Middle East Afr J Ophthalmol. 2009;16:202-18.
- [CrossRef] [PubMed] [Google Scholar]
- Intraocular manifestations of Mycobacterium tuberculosis: A review of the literature. J Clin Tuberc Other Mycobact Dis. 2017;7:13-21.
- [CrossRef] [PubMed] [Google Scholar]
- Eales' disease-current concepts in diagnosis and management. J Ophthalmic Inflamm Infect. 2013;3:11.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical features of central retinal vein occlusion with inflammatory etiology. Asia Pac J Ophthalmol (Phila). 2012;1:270-6.
- [CrossRef] [PubMed] [Google Scholar]
- Central retinal vein occlusion in a patient with retinal vasculitis and Crohn's disease. Case Rep Ophthalmol Med. 2014;2014:967878.
- [CrossRef] [PubMed] [Google Scholar]
- Combined optic neuropathy and central retinal artery occlusion in presumed ocular tuberculosis without detectable systemic infection. Ocul Immunol Inflamm. 2011;19:370-2.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of acute optic neuritis: A summary of findings from the optic neuritis treatment trial. Arch Ophthalmol. 2008;126:994-5.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of optic neuritis with intravenous megadose corticosteroids: A consecutive series. Ophthalmology. 1988;95:131-4.
- [CrossRef] [PubMed] [Google Scholar]