Translate this page into:
Role of interventional neuroradiology in ophthalmology

*Corresponding author: Shubhabrata Biswas, Department of Neuroradiology, The Walton Centre for Neurology and Neurosurgery, Liverpool, United Kingdom. drbiswas77@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Biswas S, Puthuran M. Role of interventional neuroradiology in ophthalmology. J Ophthalmic Res Pract. 2024;2:3-5. doi: 10.25259/JORP_16_2024
Interventional Neuroradiology, also referred to as Neurointervention, Neurointerventional Surgery, Interventional Neurology, Endovascular Neurosurgery, etc., has emerged over the past few decades as the preferred subspecialty dedicated to the treatment of a wide variety of neurovascular conditions. The earliest record of a neurointerventional procedure is probably traced back to the 1920s when Portuguese Neurologist Egas Moniz, along with his associate, Pedro Almeida Lima, performed the first cerebral angiography.[1,2] In the 1990s, there were landmark procedural and engineering innovations, particularly in the treatment of cerebral aneurysms with detachable coils. In the past couple of decades or so, endovascular treatment has emerged as the standard treatment for intracranial aneurysms and ischemic stroke secondary to large vessel occlusion.[3] Neurointerventional treatment is currently available for many other conditions, such as carotid stenosis, cerebral arteriovenous malformation (AVM), dural arteriovenous fistula, venous sinus stenosis, spinal vascular conditions, and tumor embolization. These therapeutic successes have been made possible by explosive advancements in technology related to the development of catheters/microcatheters, wires, coils (and other embolization or occlusion devices), stents, etc., complemented by parallel advancements in angiography, computed tomography, and magnetic resonance imaging systems.
Ocular symptoms may be the main presentation in several neurovascular conditions. The ophthalmologist may be the first point of contact for patients presenting with cranial nerve palsy secondary to an aneurysm (namely, posterior communicating artery or cavernous internal carotid aneurysm). Once an aneurysm is confirmed by imaging, endovascular treatment, namely aneurysm occlusion with coils, maybe the most appropriate treatment option. More recent advances in aneurysm treatment include stent-assisted coiling, flow diverters, and intrasaccular flow disruptors.[4]
The constellation of ocular conditions, from proptosis to ophthalmoplegia, chemosis to glaucoma, can be attributed to an underlying caroticocavernous fistula (CCF). Endovascular treatment of CCF was one of the very early endovascular therapeutic procedures attempted. In 1970, Fedor Serbinenko, a Russian neurosurgeon, performed balloon occlusion of the internal carotid to treat CCF.[2,3] The principle of treatment is to obliterate fistulous communications between the artery and the venous structure through transarterial or transvenous routes using coils or embolic materials. (e.g., acrylic glue or ethylene vinyl alcohol copolymer-Onyx, etc.). In case of a difficult venous approach, an arterialized and dilated superior ophthalmic vein (SOV) can be cannulated to approach the cavernous sinus. In our institute, this is made possible by an ophthalmic surgeon establishing the SOV cannulation through an eyelid or eyebrow incision – an excellent example of Neuroradiology and Ophthalmology collaboration [Figure 1].
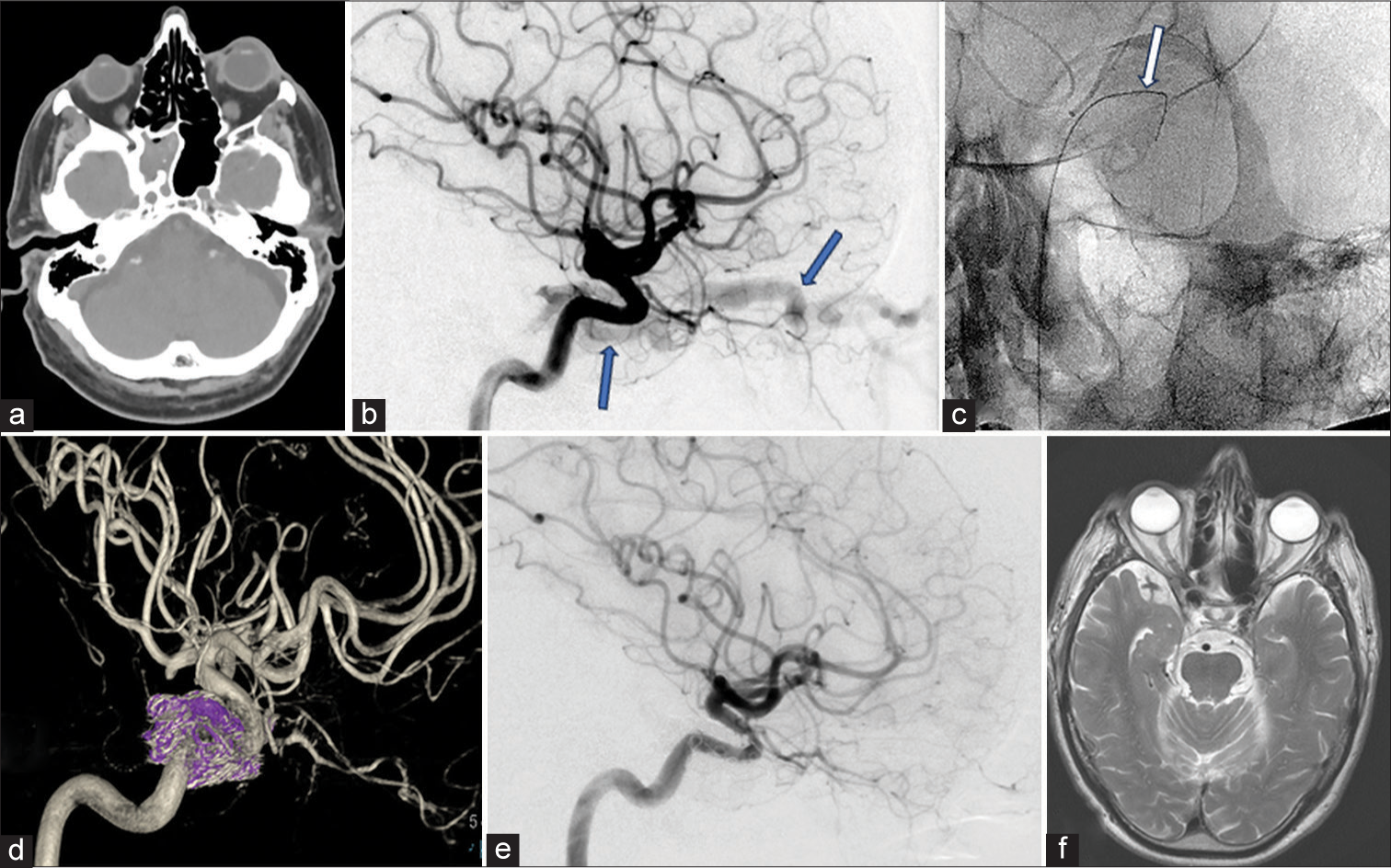
- Caroticocavernous fistula (CCF) pre- and post-endovascular treatment. (a) Computed tomography of the head showing left-sided proptosis. (b) Left internal carotid angiogram (lateral view) showing early filling of contrast in the left cavernous sinus and a dilated left superior ophthalmic vein (SOV), both indicated by blue arrows, in keeping with an underlying fistula. (c) Wire (white arrow) in the left SOV introduced externally to access the cavernous sinus. Access to the sinus through the internal jugular vein/inferior petrosal sinus was not possible in this case. Cannulation of SOV was performed by an ophthalmic surgeon by skin crease incision and open cut down. (d) Post-treatment left internal carotid angiogram (3-D spin reformat) showing occlusion of CCF with coils (in purple) in the cavernous sinus. (e) Left internal carotid artery angiogram (lateral view) post-treatment. The early filling of the cavernous sinus and SOV present previously (cf. B) is no longer seen, indicating occlusion of the fistula. (f) Magnetic resonance imaging of the head after about six months shows complete resolution of the left proptosis.
Homonymous visual field defects may be a presenting feature of a cerebral AVM. Treatment options include endovascular, surgical, or radiosurgical – one or any combination of the above. In carefully selected patients, primary endovascular embolization may be the most favorable option for treating a cerebral AVM.[5]
A patient may present to an ophthalmologist initially with visual disturbances and headaches, eventually leading to the diagnosis of idiopathic intracranial hypertension (IIH). Venous sinus stenting has been shown to be a safe and effective treatment modality to reduce headaches, papilledema, and tinnitus in medically refractory IIH.[6]
Stenting of a significantly stenosed internal carotid artery (ICA) is a routine procedure in most neurointerventional units. The corresponding author’s earliest tryst with neurointervention was about 18 years ago by observing an ICA stenting on a patient presenting with visual symptoms only (recurrent episodes of amaurosis fugax). Huge strides have been made in microcatheter technology and techniques for superselective cannulation of small caliber vessels. Ophthalmic artery cannulation and targeted delivery of chemotherapy for retinoblastoma is now a widely accepted treatment modality.[7] Novel therapeutic maneuvers, such as ophthalmic artery angioplasty for age-related macular degeneration have been reported in the literature.[8]
The examples stated above illustrate the immense value of Interventional Neuroradiology in the treatment of neurovascular conditions with ocular manifestations. However, a satisfactory treatment outcome calls for close liaison among Ophthalmologists, Interventional Neuroradiologists, Neurologists, Neurosurgeons, and other specialists. In geographical areas with limited healthcare resources, access to robust neurointerventional services may be limited. Nevertheless, referral, real-time transfer of information, and formulation of treatment pathways can be conducted effectively and efficiently through online multidisciplinary meetings with tertiary Neurosciences centers where endovascular procedures are performed routinely. High costs associated with interventional therapies can pose a major challenge. Again, costs may be low at centers where a high volume of procedures is performed. Government interventions such as limiting duties and taxes related to the trade of endovascular devices may contribute significantly. Self-reliance is an important element in securing sustainability. Atmanirbharta in manufacturing high quality devices may go a long way in making complex endovascular therapies affordable and more freely available.
References
- Neurointerventional radiology: History, present and future. J Radiol Oncol. 2023;7:26-32.
- [CrossRef] [Google Scholar]
- Interventional neuroradiology. 2024. Wikipedia. Available from: https://en.wikipedia.org/wiki/interventional_neuroradiology [Last accessed on 2024 Apr 28]
- [Google Scholar]
- Neurointervention in the 2020s: Where are we going? Clin Neuroradiol. 2021;31:1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Comprehensive review of the recent advances in devices for endovascular treatment of complex brain aneurysms. Br J Radiol. 2022;95:1129.
- [CrossRef] [PubMed] [Google Scholar]
- Primary endovascular embolisation of intracranial arteriovenous malformations (AVM)-UK single centre experience. Neuroradiology. 2024;66:227-36.
- [CrossRef] [PubMed] [Google Scholar]
- Venous sinus stenting for idiopathic intracranial hypertension: A systematic review and meta-analysis. J Neurointerv Surg. 2019;11:380-5.
- [CrossRef] [PubMed] [Google Scholar]
- The evolving role of intra-arterial chemotherapy in adult and pediatric cancers: A comprehensive review. Cureus. 2023;15:e46631.
- [CrossRef] [Google Scholar]
- Ophthalmic artery angioplasty for age-related macular degeneration. J Neurointerv Surg. 2022;14:968-72.
- [CrossRef] [Google Scholar]