Translate this page into:
Topiramate: Connecting dot of acute angle closure with myopic shift and missing link with acute anterior uveitis

*Corresponding author: Agrima Bhatia, Department of Ophthalmology, 5 Air Force Hospital, Jorhat, Assam, India. agrimabhatia123@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhatia A, Kumar S. Topiramate: Connecting dot of acute angle closure with myopic shift and missing link with acute anterior uveitis. J Ophthalmic Res Pract. 2024;2:15-8. doi:10.25259/JORP_38_2023
Abstract
An interesting case of a 38-year-old male who presented with bilateral, sudden onset, painful diminution of vision. He had raised intraocular pressure (IOP), Oculus Uterque (OU) and bilateral acute onset myopia. Ultrasound biomicroscopy (UBM) revealed bilateral (B/L) ciliochoroidal effusion. This made us revisit his history to justify the acute onset myopia associated with raised IOP, which was established to be Topiramate (TPM) induced. Fourteen days after withdrawal of TPM, he also developed unilateral acute non-granulomatous anterior uveitis that was managed conservatively. Finally, his uncorrected visual acuity was 6/6 OU, and IOP was normal without any drugs. This case illustrates the significance of meticulous history and a step-wise approach to clinch the diagnosis. It is also imperative for clinicians to recognize these conditions and educate patients about the serious adverse effects when prescribing TPM.
Keywords
Topiramate
Ciliochoroidal effusion
Myopia
Uveitis
INTRODUCTION
Topiramate (TPM) is a sulfa-derivative monosaccharide with several mechanisms of action, mainly including blockage of voltage-gated sodium channels, hyperpolarization, and enhancement of postsynaptic gamma-aminobutyric acid receptor activity.[1] It is used for a plethora of indications apart from just migraine prophylaxis, and its use has significantly increased over the past years.[2] It is, therefore prudent to know its side effects, particularly ophthalmic side effects. Although acute angle closure with myopic shift is now a documented side effect, there are still very few reported cases in the literature. Bilateral acute anterior uveitis is also a documented but extremely rare side effect of this drug.[3] Our case is unique in nature as the patient developed unilateral acute anterior uveitis on withdrawal of TPM, which has not been reported so far, hence this case report.
CASE REPORT
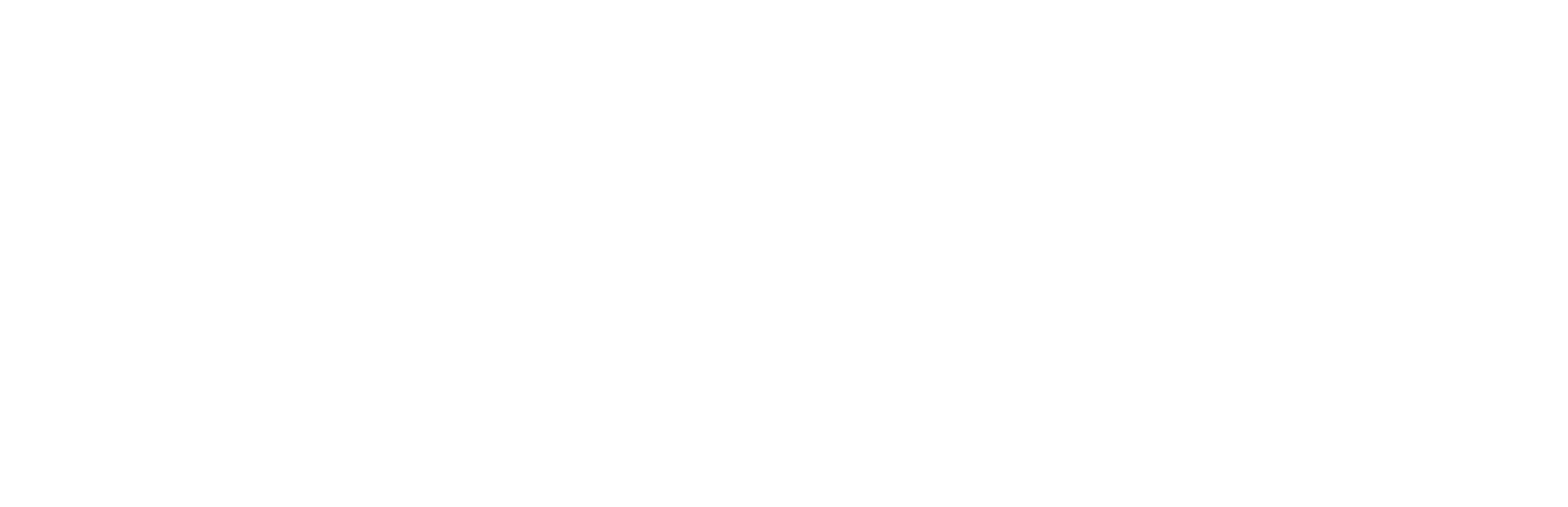
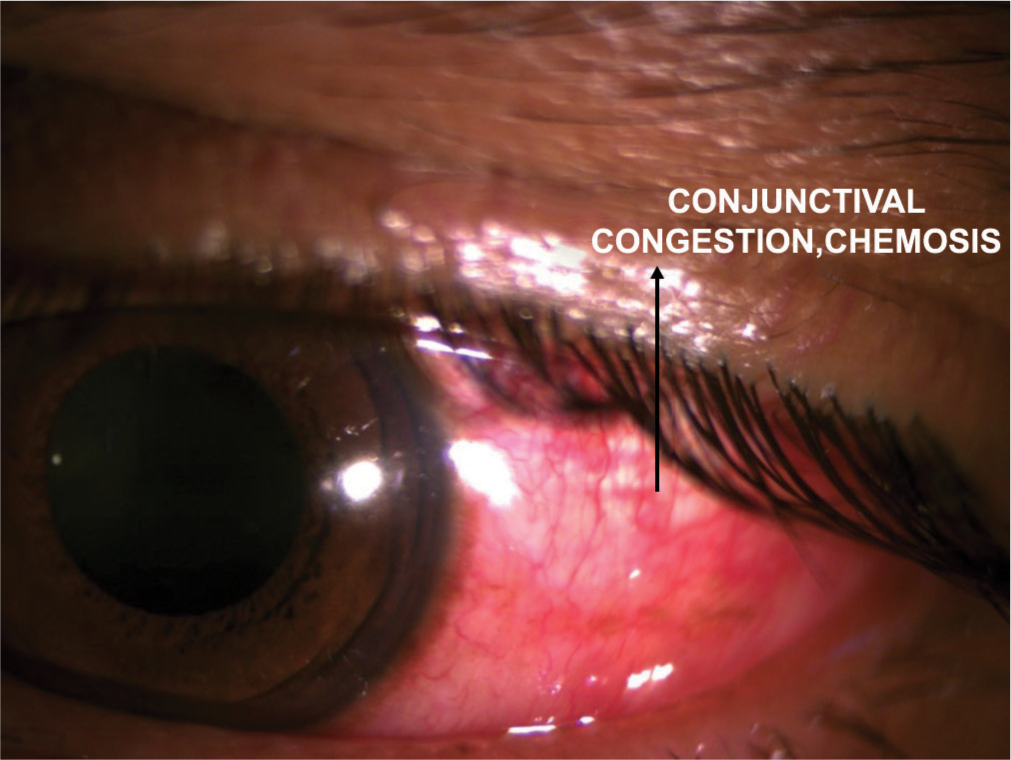
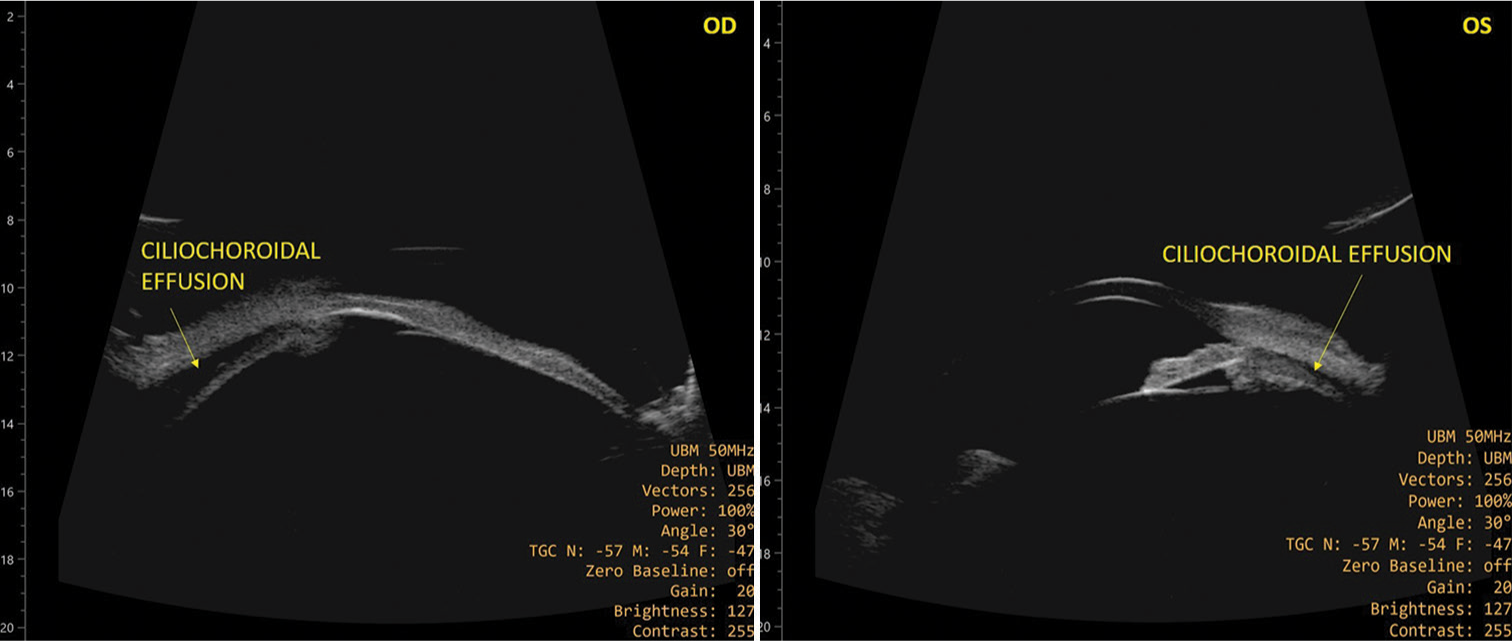
A 38-year-old male, driver by profession, with no known comorbidities presented to our eye department 24 hours (h) after he experienced sudden onset, painful diminution of vision in both eyes. He gave a history of persistent, right-sided headache for 14 days. On asking leading questions, he revealed that he was taking treatment from a practitioner for the same since two weeks that included Naproxen, TPM 25 mg once a day OD. His uncorrected visual acuity (UCVA) was 3/60 OU. Best-corrected visual acuity (BCVA) was 6/6 OU with –5.50 diopter sphere (DS). IOP with Goldmann applanation tonometry was found to be OD– 60 mm Hg and OS– 50 mm Hg. Anterior segment evaluation revealed diffuse conjunctival congestion [Figure 1], significant chemosis, shallow anterior chamber (AC) OU. Pupil was central, circular, sluggishly reacting to light. Posterior segment evaluation revealed normal fundus. Gonioscopy revealed occludable angle OU. Axial length measured for both eyes was found to be 22.86 mm and 22.85 mm. Ultrasound biomicroscopy (UBM) done revealed ciliochoroidal effusion in both eyes [Figure 2]. He was administered 350 mL of 20% IV Mannitol and two tablets of 250 mg acetazolamide stat. He was then continued on 250 mg acetazolamide BD for three days. He was also started on eye drops 0.5% Timolol 1 drop BD, 0.2% Brimonidine 1 drop TDS, and 1% Brinzolamide TDS. The rest of the treatment was discontinued. On day two of treatment, his IOP settled to 11 mmHg OU. BCVA was 6/6 OU with the same refraction. The patient was followed up regularly and on day seven, his UCVA was 6/6 OU, IOP 10 and 11, respectively, without anti-glaucoma drugs. Anterior and posterior segment evaluation was within normal limit (WNL). On day 14, the patient again reported this time with right eye redness and photophobia. On evaluation, his UCVA was 6/6 OU, IOP was 11 mmHg OU. Anterior segment evaluation of the right eye revealed circumcorneal congestion, 2 + cells in AC [Figure 3], and miotic pupil. Diagnosis of acute anterior uveitis was established, and the patient was started on e/d Prednisolone QID and 2% Homatropine BD for one week, to which he responded well. He was investigated to rule out systemic causes of uveitis and was negative for inflammatory or autoimmune diseases. On the last follow-up visit, the patient was asymptomatic with UCVA of 6/6 OU and normal IOP.
- Conjunctival congestion and chemosis (black arrow).
- Ciliochoroidal effusion detected on ultrasound biomicroscopy, OD: ocular dexter, OS: oculus sinister.
- Acute anterior uveitis showing cells in anterior chamber, developed on day 10 after Topiramate withdrawal.
DISCUSSION
The patient’s clinical presentation with high IOP and refractive error clearly pointed towards the diagnosis of acute angle closure with bilateral acute onset myopia. He was a driver by profession and had never complained of difficulty with distance vision. Hence, we confirmed it by checking his axial length, which was found to be normal. This implied that the bilateral myopia was acute in onset. Since we were unable to explain acute onset bilateral high myopia with acute angle closure, we performed UBM to determine the cause. On UBM, we elicited ciliochoroidal effusion, which made us revisit his history. He stated the fact that he had been consulting a physician who prescribed him a multitude of medicines for migraine, of which one was TPM 25 mg OD. We discontinued TPM and started him on oral acetazolamide 250 mg BD after a stat dose of 350 mL of 20% IV Mannitol and two tablets of 250 mg acetazolamide. He was also started on eye drops 0.5% Timolol 1 drop BD, 0.2% Brimonidine 1 drop TDS, and 1% Brinzolamide TDS, which settled his IOP. Thereafter, on his regular follow-up visits, his UCVA and IOP were monitored; the former took a week to normalize, and the latter was WNL after a day. His UBM was repeated after 10 days and was found to be WNL.
Although the exact mechanism of TPM-induced acute angle closure with myopic shift has not been completely understood, there are several mechanisms that have been proposed to suggest possible triggers. Sen et al. proposed one of the earliest hypotheses suggesting that entry of TPM into the lens alters its osmotic status, causing it to swell and, consequently, resulting in angle closure glaucoma (ACG) and myopia.[4] Hypothesis by Ikeda et al. in 2002 led to the origin of the clinical entity “Ciliochoroidal effusion syndrome”,which is defined as a spectrum of clinical manifestations ranging from TPM-induced transient myopia to severe bilateral ACG.[5] These were attributed to ciliochoroidal effusion and swelling of the ciliary body that can potentially result in anterior rotation of the ciliary processes, causing narrowing of the ciliary sulcus and forward displacement of the iris and lens. In TPM-induced ACG (TiACG), the uveal effusions reported are typically anterior, causing shallowing of the AC, but few cases of posterior effusion have also been found.[6] Weak carbonic anhydrase inhibitor activity, elevated prostaglandin levels, and changes in membrane potential leading to fluid movement could be implicated.[7] Large choroidal effusions from other causes are often associated with lower IOP, which may be associated with aqueous hypersecretion or ciliary body detachment.[8]
Another theory is that ciliochoroidal effusion syndrome is due to an idiosyncratic reaction. Fraunfelder et al. reviewed 115 reports of TiACG and found that 85% of cases occurred within the first two weeks of treatment and also showed that almost 50% of cases occur with doses of 50 mg or less.[9] The mean plasma elimination half-life of the drug is about 21 h; so usually, rapid visual recovery occurs, although in some cases, it may take several weeks. The principal step in the appropriate management of TiACG is making a correct diagnosis, and the most critical measure is to discontinue TPM and look for an alternative prophylaxis.
Other sulfa-based drugs, such as acetazolamide, hydrochlorothiazide, and cotrimoxazole have been associated with secondary ACG.[10]
Goldberg et al. reported seven cases of TPM-associated uveitis after a cumulative review of cases from a global safety database and published literature.[11] Of the documented cases of uveitis, cross-reactivity to sulfa-analog drug was suggested as a proximate cause. This was consistent with our case as we too, had prescribed acetazolamide to bring down the IOP, which could have elicited an inflammatory cross-reactivity. As per our literature review, no unilateral case of TPM-associated uveitis has been reported, which is why our case is unique in nature.
CONCLUSION
This case illustrates the significance of meticulous history and stepwise approach to clinch the diagnosis. It is, therefore, reinforced that clinicians recognize these conditions and educate patients about the serious adverse effects when prescribing TPM.
Ethical approval
The Institutional Ethics Committee approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Topiramate-induced acute onset myopia: A case report. BMC Res Notes. 2014;7:665.
- [CrossRef] [PubMed] [Google Scholar]
- Topiramate-associated worsening symptoms in a patient with familial hemiplegic migraine. J Neurol Sci. 2008;272:194-5.
- [CrossRef] [PubMed] [Google Scholar]
- Topiramate induced bilateral hypopyon uveitis and choroidal detachment: A report of two cases and review of literature. BMC Ophthalmol. 2021;21:287.
- [CrossRef] [PubMed] [Google Scholar]
- Case reports and small case series: Topiramate-induced acute myopia and retinal striae. Arch Ophthalmol. 2001;119:775-7.
- [Google Scholar]
- Ciliochoroidal effusion syndrome induced by sulfa derivatives. Arch Ophthalmol. 2002;120:1775.
- [Google Scholar]
- Refractory topiramate-induced angle-closure glaucoma in a man: A case report. J Med Case Rep. 2011;5:33.
- [CrossRef] [PubMed] [Google Scholar]
- Choroidal effusion and hemorrhage In: Shaarawy T, ed. Glaucoma. Philadelphia, PA: Saunders/Elsevier; 2009. p. :195-203.
- [Google Scholar]
- Bilateral angle-closure glaucoma and ciliary body swelling from topiramate. Arch Ophthalmol. 2001;119:1721-3.
- [Google Scholar]
- Topiramate-associated acute, bilateral, secondary angle-closure glaucoma. Ophthalmology. 2004;111:109-11.
- [CrossRef] [PubMed] [Google Scholar]
- Drug-induced acute angle closure glaucoma. Curr Opin Ophthalmol. 2007;18:129-33.
- [CrossRef] [PubMed] [Google Scholar]
- Is uveitis associated with topiramate use? A cumulative review. Clin Ophthalmol. 2016;10:1467-70.
- [CrossRef] [PubMed] [Google Scholar]