Translate this page into:
Premium multifocal intraocular lens: Pearls and practices

*Corresponding author: M. Vanathi, Department of Cornea and Ocular Surface, Cataract and Refractive Services, Dr R P Centre All India Institute of Medical Sciences, New Delhi, India. mvanathi.rpc@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vanathi M, Kumari P. Premium multifocal IOLs: Pearls and practices. J Ophthalmic Res Pract 2023;1:57-63. doi: 10.25259/JORP_32_2023
Abstract
Cataract surgery has gradually evolved from being a visual restoration surgery to a refractive surgery. Patients are gradually shifting from traditional intraocular lens (IOL) to high end premium IOL which provide reduced spectacle dependence and in turn greater patient satisfaction. However, these premium lenses are not without cons and calls for meticulous pre-operative calculation, realistic counseling, and perfect surgical technique. This in-depth review provides insight into the varieties of multifocal IOL, selection criteria, pre-operative planning and calculation, surgical technique, and comprehensive post-operative complication management.
Keywords
Premium intraocular lens
Multifocal intraocular lens
Extended depth of focus lens
INTRODUCTION
Cataract surgery is the most frequently performed ophthalmic surgery in the present era with high demands of post-operative visual restoration to emmetropia. The most favored choice for cataract patients who are presbyopic is premium multifocal intraocular lens (IOL). These lenses provide reduced dependence on spectacle and increase the postoperative quality of life. Sufficient pre-operative planning and clinical evaluation are critical for a successful outcome after the surgery.
Compared to traditional IOL, premium IOLs render better visual outcome but till now there is lack of standard criteria about usage of premium IOL. Premium lenses can be categorized into three groups depending on physical properties and optical design. These are accommodative IOLs, multifocal IOLs (MFIOLs), and extended depth of focus (EDOF) IOLs.[1]
Accommodative IOLs
Accommodative IOLs are designed in such a way that optics of this lens is dynamic. It can change its position, refractive index, or shape by accommodation on ciliary muscle contraction. Few accommodative IOLs designs are: Single-optic, double-optic, and deformable optic IOLs. Accommodative IOL with single-optic (Crystalens, Bausch and Lomb; 1CU, Human Optics) has hinged design between optic and haptic to enable the movement of lens anteriorly when there is pressure on the capsule bag and vitreous during accommodation. Dual-optic accommodative IOL contains a higher powered anteriorly placed IOL which is mobile and attached to a negatively low powered posterior IOL. Synchrony IOL Abbott Medical Optics (AMO), possess a positive power biconvex front lens (+32D) which is attached to a negative power concavo-convex lens. During accommodation distance between the two optics increases which in turn increases the overall effective power of the lens. These IOLs do not cause loss of contrast sensitivity or dysphotopsia but all these lenses are not devoid of limitations as they are unable to generate adequate accommodative powers.[2]
MFIOLs
MFIOLs provide spectacle independence post-cataract surgery as it can refract (or diffract) light coming from both far and near object simultaneously. Action of MFIOLs is not dependent on ciliary body function. Conventional “multifocal” IOLs were bifocal, and created a focus both for distance and near. Latest trifocal IOLs provide an extra focus for intermediate vision. These lenses can be classified depending on their mode of action, as follows:
Refractive type
These lenses possess concentric zones of various refractive powers or curvatures which enable focus for near and far objects. It correspondingly focuses light at more than one principal focus. Most common design preferred is the rotationally symmetrical lens with multiple concentric rings. They depend on pupillary size to utilize the specific zone of the lens. There are certain limitations with this lens which includes a high incidence of glare and halos symptoms due to more transition areas, intolerance to decentration of pupil, large angle kappa, and decreased contrast sensitivity. Other design is the asymmetric one which is sectoral and is similar to C-shaped bifocal glasses.[3]
Diffractive type
They have concentric rings over the entire surface with discrete borders which creates a diffractive pattern. These IOLs depend on the principle that each point of wavefront can be considered as being its own secondary wavelets manufactured with micro steps on its surface with phase delay, following the Huygens-Fresnel principle. The sum of these wavelets is the amplitude of the optic field. When light falls on those surfaces, it is divided into two foci (each 41%) for distance and near, about 18% of light is lost to higher order aberrations (HOA). It can be classified as fully diffractive and partially diffractive MFIOLs. These lenses provide an excellent reading vision with a good distance vision and they are less dependent on pupillary size and angle kappa. Few diffractive MFIOLs utilize the technology of apodization, wherein there is gradual deduction in height of diffractive step as we move toward periphery from center which causes progressive shift of light energy toward far foci making the lens distance dominant when pupillary size is large; it also reduces the symptoms of dysphotopsia.[4,5]
Extended depth of focus/range of vision IOLs (EDOF/ EROV)
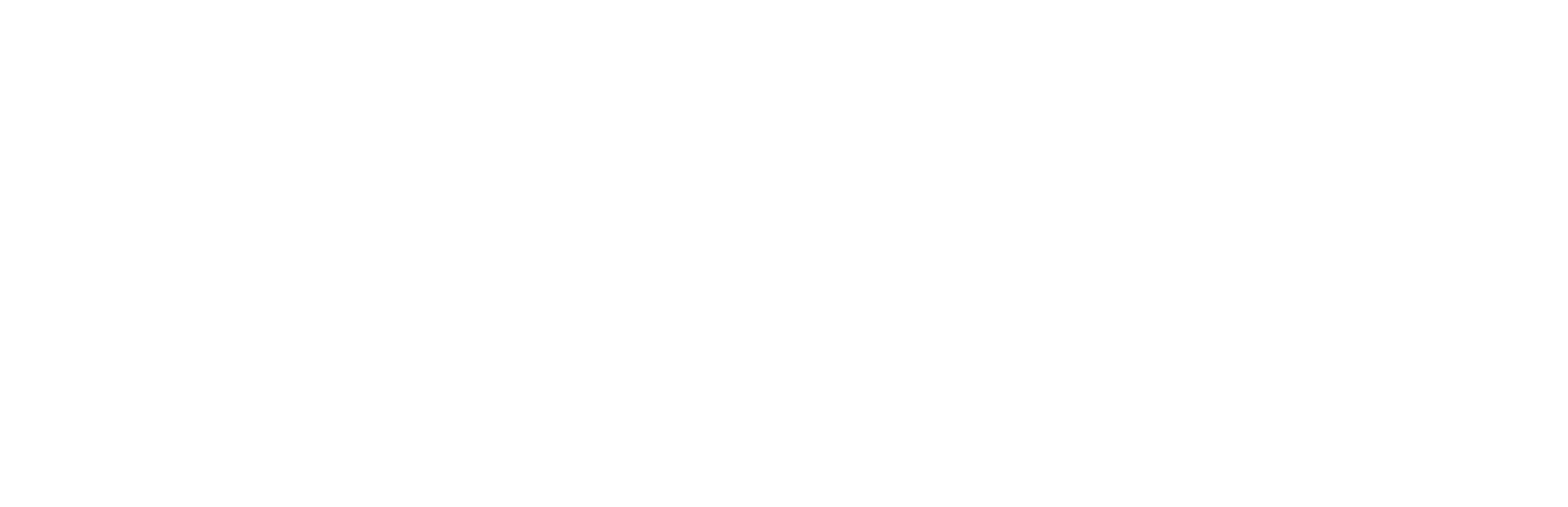
EDOF IOLs are the latest generation of IOLs that combine a unique diffractive pattern with achromatic technology, which targets to provide an elongated focus of vision. It can diminish symptoms of photopsia, glare, and halos, which were the main concern reported with conventional MFIOLs. The first EDOF lens which received U.S. Food and Drug Administration approval in 2016 was Tecnis Symfony IOL (AMO) [Figure 1]. The main optical property is the central part of the lens with an “echelette pattern” design which creates an elongated focus. The material and shape of the lens are designed to correct both chromatic and spherical aberration. In clinical practice, EDOF lenses offer superb intermediate vision, but quality of vision for near and distance is inadequate.[6]
- Tecnis Symfony as first presbyopia correcting extended depth of focus intraocular lens (IOL).
PATIENT SELECTION AND PLANNING
The importance of proper counseling in pre-operative planning for patient opting for MFIOL cannot be overemphasized. The choice of lens is decided depending on the patient’s primary ocular clinical situation, personality, lifestyle, and expectations. While making the choice, patient’s age, job profile, lifestyle requirement, hobbies, need of nighttime driving, and psychology need to be considered. Younger patients with positive personality and understanding tend to neuroadapt early hence able to tolerate minimal loss of contrast sensitivity and glare and are generally more satisfied. Patients should be educated enough about the mechanism of neuroadaptation as glare and haloes are more during nighttime driving. They must be acceptable to the fact that these symptoms usually subside with time; though neuroadaptation may take as much as 3 months to 1 year. It is pertinent to offer sufficient counseling about the possibility of a loss of contrast and temporary night time dysphotopsia but with the added advantage of wide range of vision postoperatively. Patients who have unrealistic expectations and overtly analytical personality should be avoided. Those who already have night vision problem, night work, and driving at night will have further reduction in contrast sensitivity. Hence, MFIOLs are mostly recommended for subjects who are highly motivated for reduced spectacle dependence, and are willing to tolerate certain amount of dysphotopsia in the initial phase.[7,8]
PRE-OPERATIVE OCULAR EVALUATION
Ocular surface evaluation
The first refractive surface of the eye is the tear film; any irregularity herein leads to symptoms of dysphotopsia. The most common ocular surface disease is Meibomian gland dysfunction, dry eye and blepharitis. Dry eye disease if detected preoperatively needs to be managed before surgery. Pre-operative dry eye can be a cause of postoperative refractive surprise, blurred vision, and foreign body sensation. Patients are often unhappy if they experience excessive tearing and photophobia due to dry eye.[9]
Corneal pathologies
Slit lamp examination should rule out any pathology in the cornea such as old opacity, scarring, corneal edema, corneal dystrophies, advanced pterygium, or irregular astigmatism in keratoconus. History of refractive corneal surgery should be ruled out.
Pupil size, angle kappa, and angle alpha
MFIOLs require a perfectly round and well centered pupil for good visual demands. Thus, patients with abnormalities of pupillary size or shape, namely, corectopia, iris coloboma, and iris atrophy are not ideal candidates. Patients having severe miosis do not gain good near vision, while patients having mydriatic pupils postoperatively who require mydriatic devices intraoperatively experience higher amounts of haloes and glare. Size of pupil should be evaluated in photopic, mesopic, and scotopic conditions before planning for premium IOLs. It is suggested that eyes implanted with MFIOLs should ideally have ≤3.5 mm photopic pupil size and ≤5 mm mesopic pupil size.[10]
Angle kappa (K) is defined as the angle formed between the visual axis and the pupillary axis whereas angle alpha is the angle formed between the visual axis and the optical axis. Large angle K is responsible for decentration of MFIOLs, causing glare, and halo. Well-centered lens in the visual axis is imperative for presbyopic IOLs to function well.[1]
Angle alpha is defined as the radial distance between the center of the limbus and the visual axis, which was found to predict the tilt of the IOL in respect to the visual axis. Angle alpha has emerged as better predictor for photic phenomena and patient satisfaction with MFIOLs.[1]
Capsular bag stability
Ocular conditions which might lead to capsular bag and zonular instability must be ruled out in slit lamp examination under full mydriasis. Any zonular weakness such as pseudoexfoliation may cause capsular bag and IOL decentration with IOL tilt in the future, resulting in loss of efficacy of MFIOL. If zonular dialysis or posterior capsular rupture (PCR) occurs intraoperatively then MFIOLs to be avoided and aspheric lens to be implanted.[4]
Optic nerve pathologies
Patients who are suspected of glaucoma, have ocular hypertension, or in the early stage of glaucoma with controlled intraocular pressure and stable visual field are candidates for diffractive MFIOLs and EDOF IOLs. However, patients having advanced visual field change, progressive glaucoma, or with risk of pupillary or zonular changes due to use of chronic miotics, pigment dispersion, and pseudoexfoliation are unlikely to benefit from MFIOLs as the contrast sensitivity further reduces.[11]
Retinal diseases
Diseases of the macula reduce contrast sensitivity of the eye, so implanting a MFIOL is not indicated in those patients. Routine pre-operative macular optical coherence tomography (OCT) is advisable before planning a MFIOL. MFIOLs are strictly not recommended in Stargardt’s disease and retinitis pigmentosa while relative contraindications include diabetic retinopathy, age-related macular degeneration, and epiretinal membranes.[12]
Patients with amblyopia and strabismus are also not ideal candidates for MFIOL.
PRE-OPERATIVE CALCULATION
Corneal astigmatism
The main aim of spectacle freedom is achievable if there is no or minimal residual ametropia. Accurate results are obtained by optical biometry. Newer fourth-generation formulae like Barrett’s universal II formula are most accurate.
Keratometry readings obtained from optical biometry and corneal topography must be comparable. Post-operative astigmatism of above 0.75 D can affect MFIOL efficacy adversely. The prime cause for patient’s dissatisfaction following surgery is astigmatism more than 1.5 D. High postoperative astigmatism may induce dysphotopsia symptoms which decreases visual function of MFIOLs.[8]
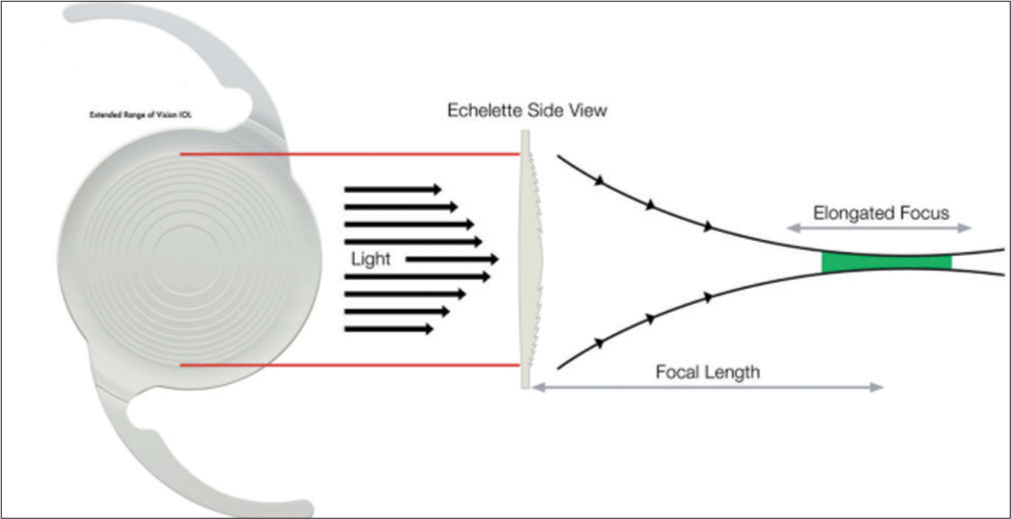
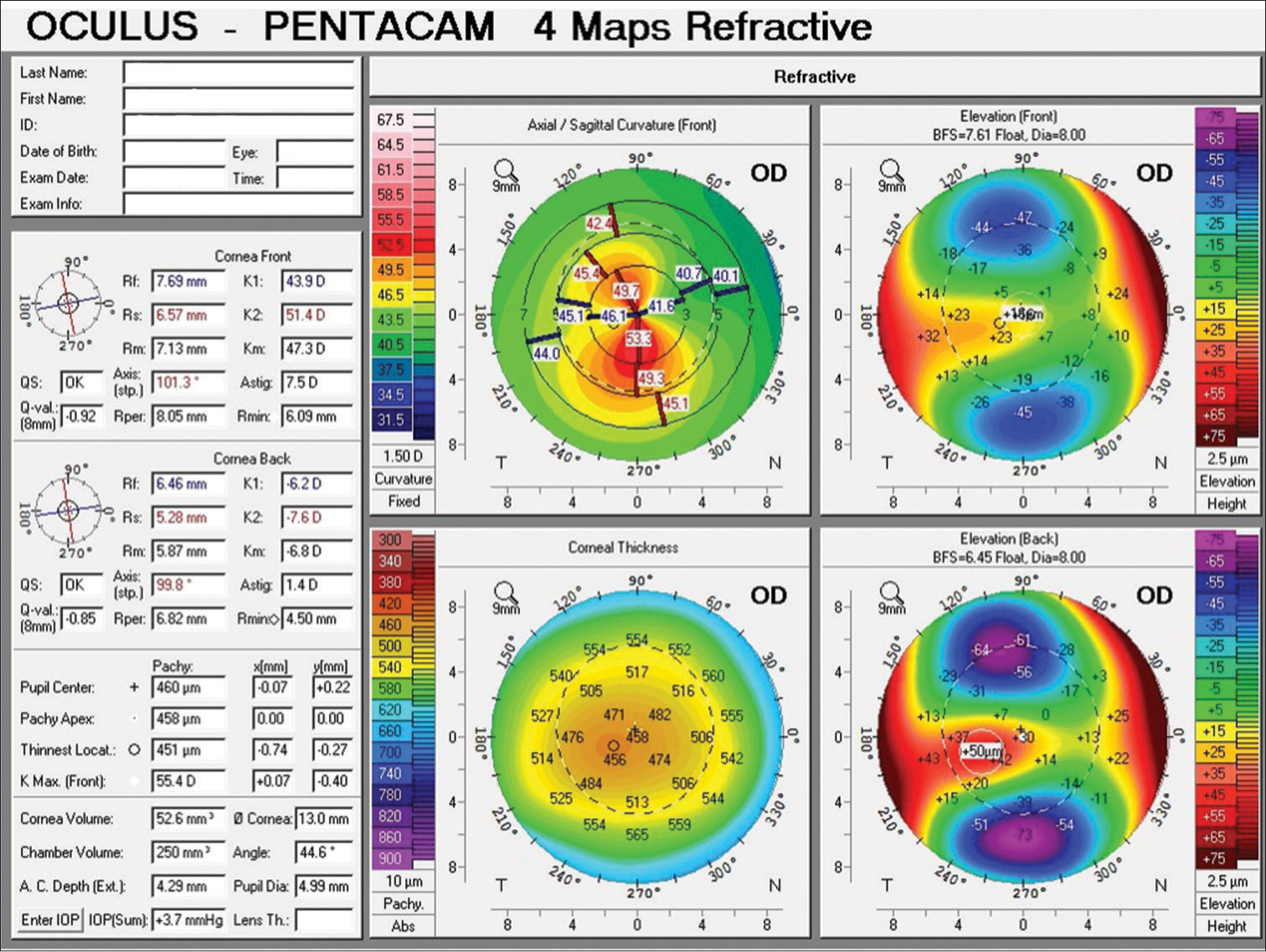
Pre-operative astigmatism can be detected by keratometry, autorefractometry, and corneal topography. This should guide the surgeon to choose the astigmatism correcting options such as limbal relaxing incisions (LRI) or toric MFIOLs. Corneal topography provides insight into the pattern of corneal astigmatism, its shape, and also helps in planning the corneal incisions. Tomography devices like Pentacam [Figure 2] or swept source OCT-based optical biometer (IOLMaster 700) can measure the posterior corneal astigmatism or total corneal astigmatism which is more accurate in estimating astigmatism in patients awaiting MFIOL implantation.[13] Most online calculators consider anterior corneal astigmatism, posterior corneal astigmatism and surgically induced astigmatism (SIA), and choose toric IOL using total corneal refractive power or in-built nomogram. Newer technologies have evolved to enhance the outcome which includes intraoperative wavefront aberrometry (ORA system, Alcon), Image Guided System like Verion (Alcon), and Callisto Eye (Carl Zeiss Meditec). In the iTrace device, corneal topography is combined with wavefront aberrometry [Figure 3].
- Pentacam four map refractive suggestive of keratoconus. OD: right eye; best fit sphere: BFS; A.C. Depth: Anterior Chamber Depth; K.Max: Maximum keratometry, IOP: Intraocular pressure; QS: Quantity sufficient; Q-val: coefficient of corneal asphericity, K1: flat meridian of the anterior corneal surface , K2- steep meridian of the anterior corneal surface; Astig: Astigmatism; Rmin: retinal microcapillary network.
- Display of map summary on wavefront aberrometry for planning of multifocal intraocular lens (IOLs). HO - higher order.
Patients who have undergone corneal refractive surgeries usually select premium IOLs with high expectation but IOL power calculation is challenging in these cases as the higher order corneal aberrations are high and increased risk of photophobia and glare is present.[1]
Ocular biometry and IOL power calculation
Accurate calculation of MFIOL powers is one of the most critical and challenging steps for delivering emmetropia to attain spectacle freedom. Achieving this goal requires eliminating astigmatism and attaining a precise plano postoperative refraction within ±0.25 D. Biometry involves measurements of Axial length (AL), keratometry, anterior chamber depth, lens thickness, and horizonal white to white diameter. Pre-operative refraction and size of pupil also affects post-operative outcome.[14]
The variables which affect IOL power calculations are keratometry reading, AL, lens power, effective lens position, desired refractive outcome, and vertex distance. The IOL design and lens positioning affects the effective lens position. Prediction of effective lens position is vital for calculating the IOL power. In addition to precise biometry, the choice of IOL power calculation formula is also crucial for success of premium IOL surgery. Third-generation formula can get accurate refractive result in eyes with normal AL and keratometry, but special attention must be paid to eyes having long AL and abnormal corneal power. Newer IOL power calculation formula such as Barrett universal II, Hill-RBF, and Olsen can deliver more precise and accurate reading in eyes with longer and shorter AL.[15]
IOL power calculation in post-corneal refractive surgery eyes presents a challenge. Recent IOL power calculation formulas, like the ascrs.org web-based calculator and Barrett True-Keratometry formula [Figure 4] furnish precise predictable refraction.[16]
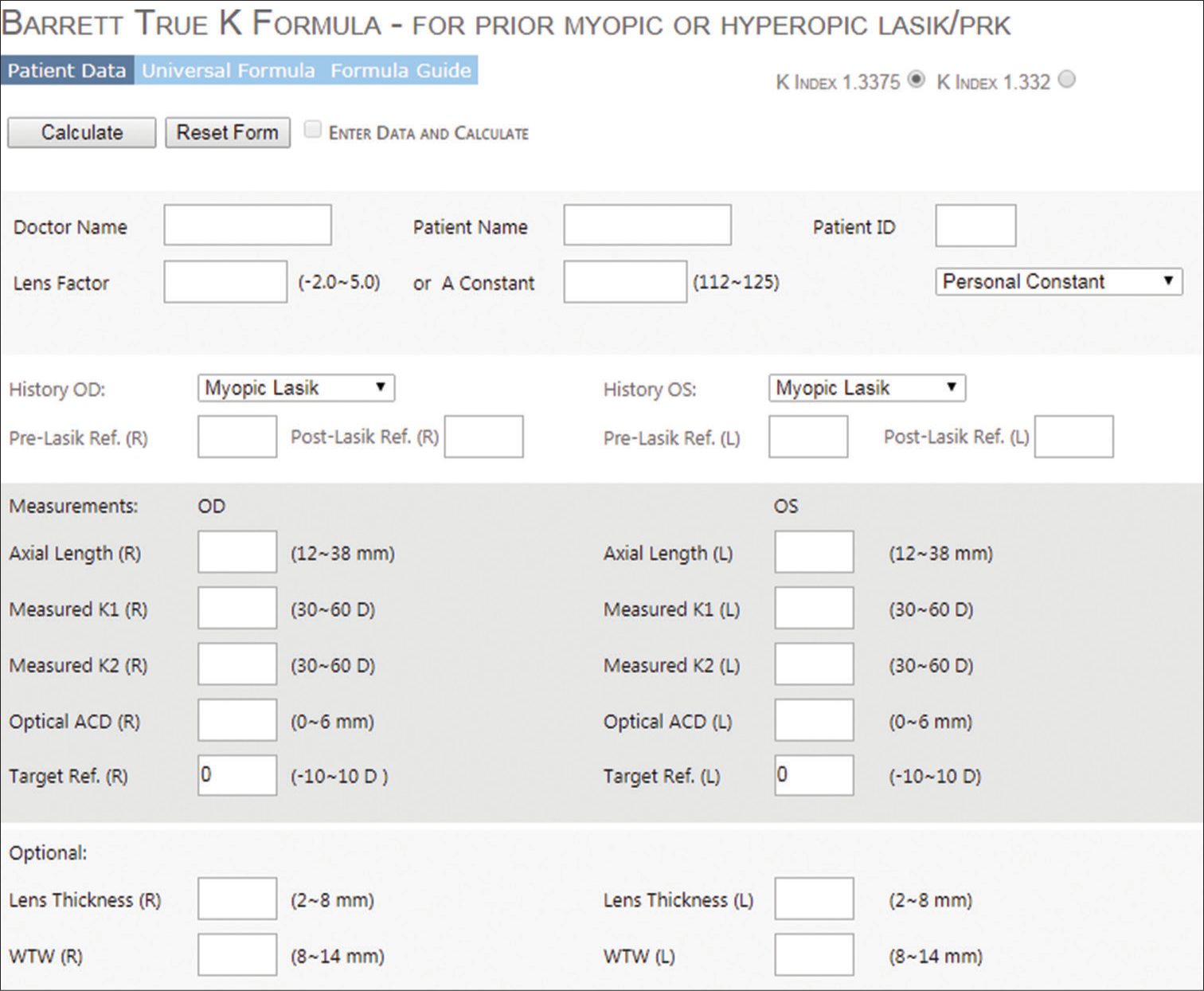
- Online Barrett True K calculator for accurate intraocular lens (IOL) power calculation; OD: right eye, OS: left eye, WTW: white-to-white; K1: flat meridian of the anterior corneal surface , K2-steep meridian of the anterior corneal surface; ACD: Anterior chamber depth.
SURGICAL TECHNIQUES
Before proceeding for a premium, IOL surgeons must pay attention to pre-operative biometry and IOL power calculation. Pre-existing or SIA can significantly affect the visual outcome. A definite pre-requisite criterion for MFIOL implantation is an uneventful surgery. For astigmatism less than 1.0 D, the incision at steep axis is the preferred approach whereas LRIs are the preferred choice for astigmatism up to 1.5 diopter. Astigmatism more than 1.5 D can be best managed with multifocal toric IOLs. For toric IOLs, corneal limbal marking is done by manual or computer-assisted automated devices. Capsulorrhexis must be central, circular, and having optimum size of 5–5.5 mm so that the lens is symmetrically overlapped 360º by the anterior capsule. In the bag implantation of the lens is a must. While implanting toric MFIOL, final alignment of lens needs to be rechecked after viscoelastic substance has been removed. Relative contra-indications for MFIOL implantation are PCR and zonular dialysis, so a three-piece monofocal IOL needs to be kept as a backup for such a situation. In case of small PCR, MFIOL may be placed if in the bag placement of IOL is possible. If zonular dialysis is small, and manageable with capsular tension rings (CTR), MFIOL may be implanted.[1,17]
POST-OPERATIVE COMPLICATIONS
Blurred vision and residual refractive error
This is the most common cause of dissatisfaction after MFIOL implantation. When the residual astigmatism or ametropia is large, patients may be offered the option of spectacle or contact lens use, laser vision correction, piggyback IOL, or IOL exchange, based on the severity of the error. Other causes of blurred vision could be due to large pupil, dry eyes, retained lens matter, and posterior capsular opacification (PCO).[18]
IOL-related complications
IOL decentration and IOL tilt are the most critical complications seen with MFIOLs. If IOL is decentered from the center then it loses its ability to achieve optimal visual outcome. Symptoms depend on the degree of decentration, IOL design, and pupillary size. Argon laser iridoplasty has been tried in these cases. IOL tilt largely depends on the material and biocompatibility of the haptics. Rotationally asymmetric refractive IOL is more sensitive to tilt due to its inherent design and characteristics. C-loop haptic design IOLs are more prone for decentration and tilt when the capsular bag starts to contract. Hence, CTR can be implanted to prevent IOL movement due to bag contraction.[19]
Posterior capsular opacity
Patients with MFIOL who develop an early PCO may experience visual problems, which calls for an early Neodymium-doped yttrium aluminum garnet (Nd:YAG) capsulotomy.[4]
Inadequate pupil size
Pupillary size after cataract surgery is an important factor which determines the IOL performance. It is directly related to the photic phenomenon postoperatively. Very small pupil size can limit the near vision performance. In this cases, use of cycloplegics and 360° argon iridoplasty has been attempted.[20]
Photic phenomenon and contrast sensitivity
Glare and halos are the top and most frequent reasons for dissatisfaction after MFIOL implantation. Glare occurs due to overall brightening of field of vision which occurs as a result of increased scattering of light by the lenses. Refractive IOL designs are more prone for this photic episode. Halos are concentric rings illuminated around the light objects caused due to HOA. When the rays of light are refracted by a MFIOL, a shadow is created on the retina in their original path of light, whereas a central area is illuminated more, leading to negative and positive dysphotopsia, respectively. Management of these symptoms starts before the surgery. Adequate pre-operative education to the patients regarding these photic phenomenon needs to be discussed. In most of the cases, mild-to-moderate photic phenomenon is seen and most of the patients get used to it with time if they are educated enough about the neuroadaptation process. Night professional drivers and patients with large scotopic pupil size are the poor candidate for MFIOL implantation.[12]
CONCLUSION
A meticulous pre-operative planning with patient education regarding all the pros and cons of premium IOL will facilitate achieving ideal outcomes postoperatively offering reduced spectacle dependence and enhanced quality of life. Surgical procedures should be optimized technically to attain the desired results. Proper counseling of patients with increased chair time will go a long way in enhancing the outcome of present premium IOLs.
Ethical approval
Not applicable.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Successful Premium Multifocal IOL Surgery: Key Issues and Pearls. In: Current Cataract Surgical Techniques. London: IntechOpen; 2021.
- [CrossRef] [Google Scholar]
- Near visual outcomes with single-optic and dual optic accommodating intraocular lenses. J Cataract Refract Surg. 2012;38:1568-75.
- [CrossRef] [Google Scholar]
- Effect of position of near addition in an asymmetric refractive multifocal intraocular lens on quality of vision. J Cataract Refract Surg. 2015;41:945-55.
- [CrossRef] [PubMed] [Google Scholar]
- Optimizing outcomes with multifocal intraocular lenses. Indian J Ophthalmol. 2017;65:1294-300.
- [CrossRef] [PubMed] [Google Scholar]
- Characterization of visual phenomena with the array multifocal intraocular lens. J Cataract Refract Surg. 2002;28:1195-204.
- [CrossRef] [PubMed] [Google Scholar]
- Defocus curves of 4 presbyopia-correcting IOL designs: Diffractive panfocal, diffractive trifocal, segmental refractive, and extended-depth-of-focus. J Cataract Refract Surg. 2019;45:1625-36.
- [CrossRef] [PubMed] [Google Scholar]
- Multifocal intraocular lenses: Relative indications and contraindications for implantation. J Cataract Refract Surg. 2014;40:313-22.
- [CrossRef] [PubMed] [Google Scholar]
- Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37:859-65.
- [CrossRef] [PubMed] [Google Scholar]
- An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Refract Surg. 2019;45:669-84.
- [CrossRef] [PubMed] [Google Scholar]
- Pupil dependence assessment with multifocal intraocular lenses through visual acuity and contrast sensitivity defocus curves. Eur J Ophthalmol. 2020;31:2989-96.
- [CrossRef] [PubMed] [Google Scholar]
- Multifocal intraocular lenses: An overview. Surv Ophthalmol. 2017;62:611-34.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of intraoperative aberrometry on the rate of postoperative enhancement: Retrospective study. J Cataract Refract Surg. 2010;36:747-55.
- [CrossRef] [PubMed] [Google Scholar]
- Calculation of intraocular lens power: A review. Acta Ophthalmol Scand. 2007;85:472-85.
- [CrossRef] [Google Scholar]
- Accuracy of intraocular lens calculation formulas. Ophthalmology. 2018;125:169-78.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the accuracy of intraocular lens power calculation formulas for eyes after corneal refractive surgery. Ann Transl Med. 2020;8:871.
- [CrossRef] [PubMed] [Google Scholar]
- Multifocal toric intraocular lenses versus multifocal intraocular lenses combined with peripheral corneal relaxing incisions to correct moderate astigmatism. J Cataract Refract Surg. 2014;40:1625-32.
- [CrossRef] [PubMed] [Google Scholar]
- Secondary procedures after presbyopic lens exchange. J Cataract Refract Surg. 2004;30:1461-5.
- [CrossRef] [PubMed] [Google Scholar]
- Decentration and tilt of plate-haptic multifocal intraocular lenses in myopic eyes. Eye Vis (Lond). 2020;7:17.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of differences in pupil size following phacoemulsification surgery. Int J Appl Basic Med Res. 2018;8:155-7.
- [CrossRef] [PubMed] [Google Scholar]