Translate this page into:
Rhino orbital mucormycosis: The new mimicker of neuro-ophthalmic lesions

*Corresponding author: Sunanda Nandi, Department of Pediatric, Strabismus and Neuroophthalmology, David Brown Children Eye Care Centre, L V Prasad Eye Institute, Vijayawada, Andhra Pradesh, India. sunanda.amc@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nandi S, Chougule P, Dam B. Rhino orbital mucormycosis: The new mimicker of neuro-ophthalmic lesions. J Ophthalmic Res Pract 2023;1:72-5. doi: 10.25259/JORP_3_2023
Abstract
It was always challenging to start steroids in a suspected optic neuritis case with rhino-orbital mucormycosis being the differentials in the COVID era. A 27-year-old female presented with headache and fever for 1 week, along with sinusitis and both eyes (BE) blurred vision for 2 days. There was history of tingling sensation in both lower limbs with urinary retention previously. History of COVID infection 1 month back. Vision in Right Eye (RE): 20/20 and Left Eye (LE): counting fingers (CF) CF with presence of relative afferent pupillary defect (RAPD) Grade 3. Humphrey Visual field gave a picture of Junctional scotoma with ganglion cell loss noted in BE. Magnetic resonance imaging (MRI) brain with orbit gave a picture of LE optic neuritis with right ethmoidal, sphenoidal sinusitis involving orbital apex making mucor a suspect. MRI spine showed focal myelitis. Patient underwent nasal endoscopy to rule out rhino-orbital mucormycosis following which she was started on intravenous methylprednisolone (IVMP) and vision improved drastically. Hence, a diagnosis of neuromyelitis optica was made. Three doses of IVMP along with a tapering dose of oral prednisolone were given and the patient is still in follow-up with no recurrence reported till now.
Keywords
Optic neuritis
Rhino orbital mucormycosis
Neuromyelitis optica
Junctional scotoma
Intravenous methylprednisolone
INTRODUCTION
In the era of COVID-19, rhino-orbital-cerebral mucormycosis became the life-threatening invasive fungal infection.[1] Its various presentation made it a mimicker of several rhino-orbital lesions making the practice of medicine more controversial. We intend to cite one of those cases in which administration of steroid for the treatment was disputable.
CASE REPORT
A 28-year-old female, student by profession, resident of Odisha reported with the chief complaints of diminution of vision in the left eye (LE) 2 days before presentation. It was sudden in onset and gradually progressive. It was associated with headache for 1 week. There was no history of trauma or any head injury. However, there was history of fever on/off for 10 days.
Patient was tested COVID positive in rapid test, 1 month back. There was history of tingling and numbness in both lower limbs with urinary retention for which she was treated 1 month back. No history of similar incidence of loss of vision in the past was reported. Family history, allergic history was not significant.
On examination
Visual acuity in the right eye (RE) 20/20 and in the LE was counting fingers. LE showed relative afferent pupillary defect Grade 3 with disc pallor. Normal Cup Disc ratio was noted in both eyes (BE). There was evidence of a total defect in color vision in LE. Extraocular movement was normal in BE as shown in Figure 1. Rest of the anterior and posterior segment was normal.

- Extraocular motility.
On investigation
Humphrey visual field showed junctional scotoma as shown in Figure 2.
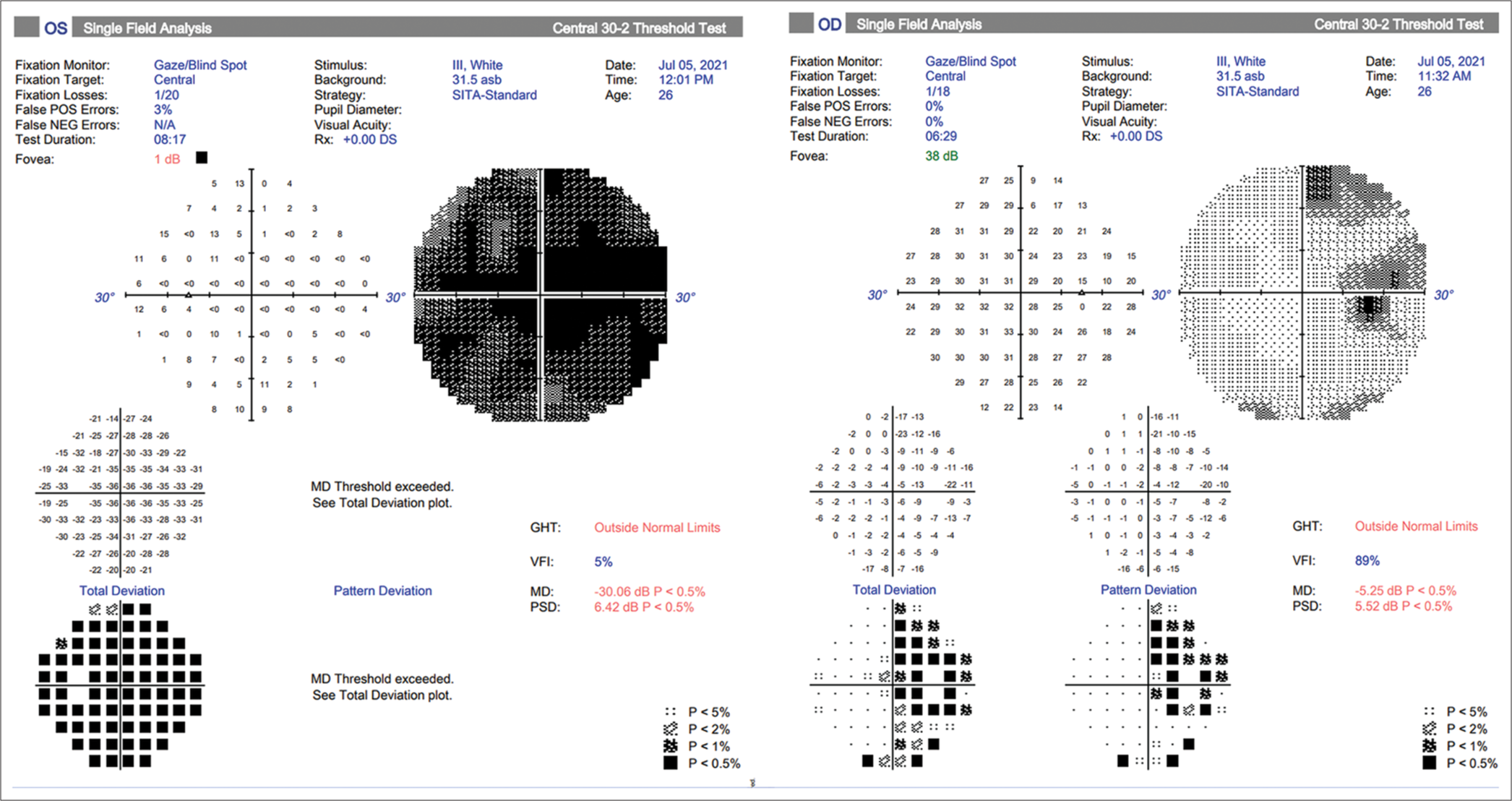
- Humphrey visual field showing junctional scotoma; POS: Positive; NEG: Negative; SITA: Swedish Interactive Testing Algorithm; DS: Dioptre spherical; Db: Decibel; MD: Mean Deviation; GHT: Glaucoma Hemifield Test; VFI: Visual Field Index; PSD: Pattern Standard Deviation.
Optical coherence tomography showed thinning of retinal nerve fiber layer and papillomacular bundle as shown in Figure 3.

- Optical coherence tomography shows thinning of retinal nerve fiber layer and papillomacular bundle; Gross percentage of population having the values marked with different colors , signifying its thickness in y axis; OD: right eye, OS: left eye, Gcl: ganglion cell layer, RNFL: retinal nerve fiber layer, T: temporal, S: superior, N: nasal, I: inferior; Red: advanced thinning; Yellow: moderate thinning; Green: normal.
MRI brain and orbit with contrast showed left optic nerve hyperintensity in T2 contrast images suggestive of LE optic neuritis as shown in Figure 4a. Coronal section showed right posterior ethmoidal sinusitis, sphenoidal sinusitis with apical enhancing irregular densities involving the chiasma which explained the junctional scotoma as shown in Figure 4b. MRI spine showed focal myelitis.
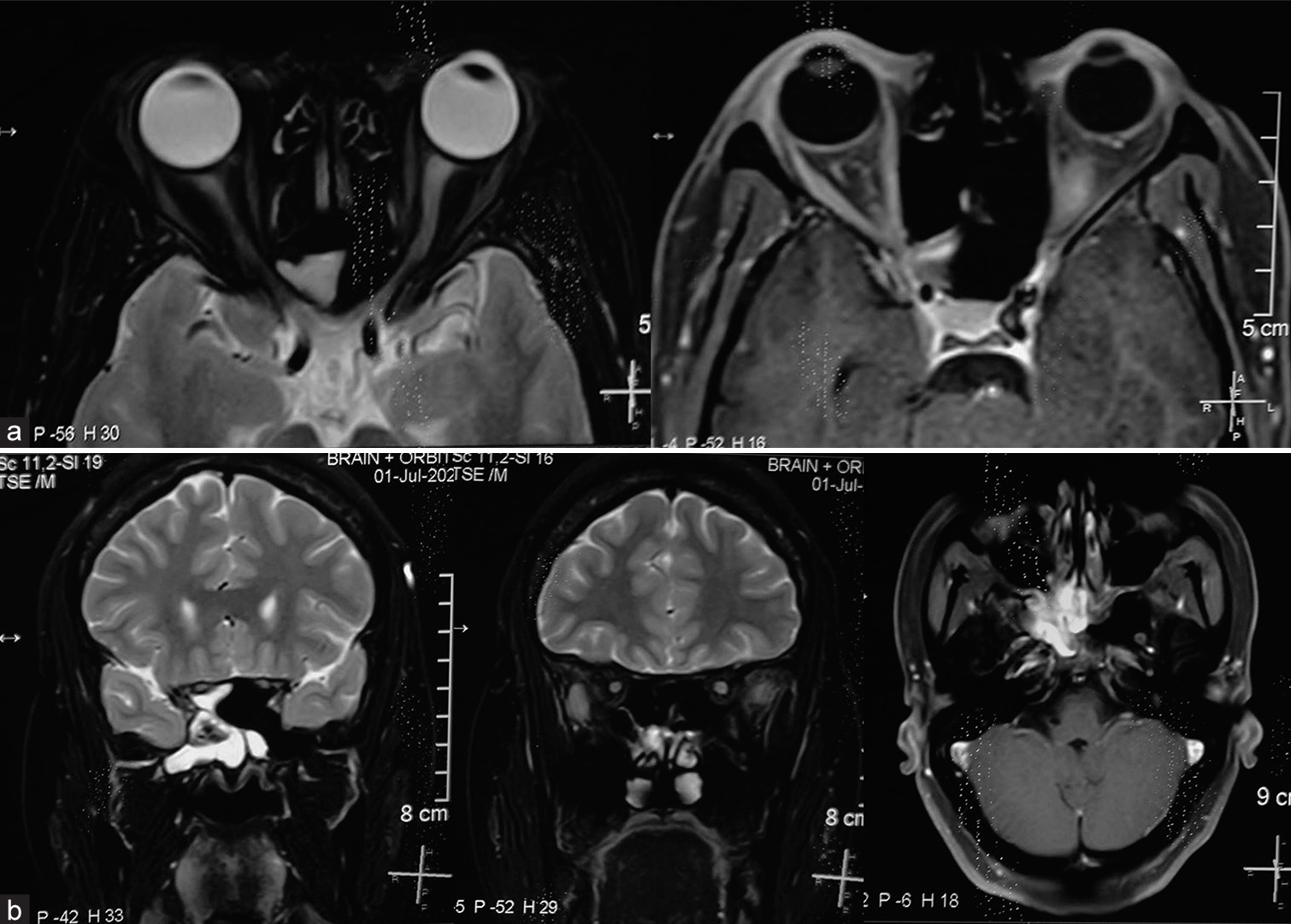
- (a) Magnetic resonance imaging brain with orbit with contrast showed left optic nerve hyperintensity in T2 contrast images suggestive of left eye optic neuritis. (b) Coronal section shows right posterior ethmoidal sinusitis, sphenoidal sinusitis with apical enhancing irregular densities involving the chiasma which explains the junctional scotoma.
Our probable diagnosis was LE atypical optic neuritis (neuromyelitis optica) versus rhino orbital mucormycosis.
Patient was referred to an ENT doctor to rule out mucormycosis. Endoscopy was not suggestive of mucormycosis. Patient was diagnosed with bilateral sinusitis involving all the sinuses.
Treatment
Patient was started on intravenous methylprednisolone 1000 mg in 100 mL saline over 30 minutes for 3 days, tablet Pantoprazole 40 mg-once daily, tablet Calcium 500 mg-once daily.
Vision improved to DAY 1: 20/800; DAY 2: 20/600, and DAY 3: 20/500.
Patient was started on oral medications and no deterioration was noted. Vision was stable at 20/400 (Log MAR +1.3) after 1 month.
DISCUSSION
Mucormycosis is a threatening and invading fungal infection that invades the orbit through lamina papyracea often extending posteriorly causing orbital apex syndrome, and affects vision when the optic nerve is involved.[2]
In a case report published by Singh et al.,[3] where they cited evidence of perineural spread of mucormycosis that caused optic neuritis, which responded to timely management and prompt intervention.
Ghuman et al.,[4] presented a rare case of mucormycosis where MRI showed bilateral optic nerve infarction and perineural extension of the fungus along the trigeminal nerve.
Shams et al.[5] reported posterior segment findings in 480 eyes of patients with post-COVID mucormycosis. Orbital involvement was seen in 151 (31.45%) cases. Out of 151, normal fundus was seen in 65 eyes, diabetic retinopathy in 26 (17.21%) eyes, central retinal artery occlusion in 22, disc pallor in 12, and disc edema in 10.
Raj et al.[6] have reported several manifestations of rhino orbital cerebral mucormycosis including ocular motility disorders, periocular sensation abnormalities, ptosis, eschar in eyelid, proptosis, subconjunctival hemorrhages, anterior segment inflammation, raised intraocular pressure, corneal edema, and abnormal pupillary reaction.
A review of 208 cases of rhino-orbital-cerebral mucormycosis published between 1970 and 1993 reported following symptoms and signs.[7]
Fever – 44%
Nasal ulceration or necrosis – 38%
Periorbital or facial swelling – 34%
Decreased vision – 30%
Ophthalmoplegia – 29%
Sinusitis – 26%
Headache – 25%
In our case, there was no evidence of invasion of optic nerve by the fungus; however, it presented as a mimicker of it. It was a case of neuromyelitis optica as she was presented with past history of bilateral limb weakness and bladder incontinence. Nasal endoscopy was normal which helped us to differentiate the case from mucormycosis, and give systemic steroids which improved the vision.
CONCLUSION
In that era of mucormycosis, steroids were dreadful like death with one misdiagnosis. History, examination aided by proper investigation, and their correct interpretation with multidisciplinary management protocols can save one’s life above sight.
Ethical approval
Not applicable.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Epidemiology and diagnosis of mucormycosis: An update. J Fungi (Basel). 2020;6:265.
- [CrossRef] [PubMed] [Google Scholar]
- MRI characteristics of neuromyelitis optica spectrum disorder: An international update. Neurology. 2015;84:1165-73.
- [CrossRef] [PubMed] [Google Scholar]
- Optic neuritis in post-Covid rhino-orbito-cerebral mucormycosis (ROCM): A rare presentation. Int J Case Rep Images. 2021;12:1-6.
- [CrossRef] [Google Scholar]
- Bilateral optic nerve infarction in rhino-cerebral mucormycosis: A rare magnetic resonance imaging finding. J Neurosci Rural Pract. 2015;6:403-4.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior segment findings in post-Covid mucormycosis: A cross-sectional study. IP Int J Ocul Oncol Oculoplasty. 2022;8:136-40.
- [CrossRef] [Google Scholar]
- A cross-sectional study to describe the spectrum of ocular manifestations and risk factors of mucormycosis presenting to a tertiary hospital of East India. Indian J Ophthalmol. 2023;71:249-56.
- [CrossRef] [PubMed] [Google Scholar]
- Survival factors in rhino-orbital-cerebral mucormycosis. Surv Ophthalmol. 1994;39:3.
- [CrossRef] [PubMed] [Google Scholar]